5414
Role of Intracranial Vessel Wall (VW) MRI in Evaluating Luminal Pathologies.1Neuroradiology, National Neuroscience Institute, Singapore, Singapore, 2National Neuroscience Institute, Singapore, Singapore
Synopsis
Intracranial vessel wall (VW) MRI is a state-of-art technology to evaluate vessel wall diseases. It requires high spatial and contrast-to-noise ratio (CNR) resolution as well as capability of blood and cerebrospinal fluid (CSF) suppression to visualize the arterial wall. Our vessel wall protocol including T2 -weighted, 3D time of flight (ToF) MR angiography, diffusion-weighted imaging (DWI), gradient echo imaging (GRE), high resolution post contrast 3D T1-weighted turbo spin echo (TSE) with motion-sensitized driven-equilibrium (MSDE) black blood sequence and post contrast 3D T1-weighted volumetric isotropic fast field echo (FFE) done within 30 minutes which is capable to show vessel wall diseases.
Background
Intracranial vessel wall (VW) MRI is a state-of-art technology to evaluate diseases within the wall of the arteries, beyond the luminal anomalies demonstrated on angiographic images. The imaging of vessel walls allows characterization of atherosclerosis, vasculitis, dissections and moya-moya disease which will impact the treatment decisions made. In order to visualize the thin arterial walls, vessel wall imaging requires high spatial and contrast-to-noise ratio (CNR) resolution as well as capability of blood and cerebrospinal fluid (CSF) suppression which are challenging within a tolerable acquisition time so that motion artefacts can be reduced.Teaching Points
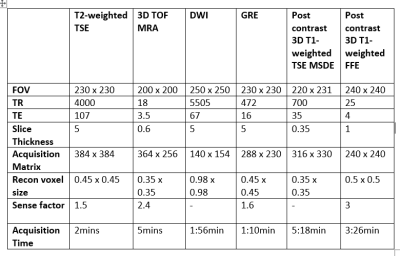
Intracranial vessel wall MRI is predominately performed on a 3 Tesla MRI Philips Ingenia system (Philips Healthcare, Best, the Netherlands) with a 32-channel head coil in Neuroradiology, National Neuroscience Institute, Singapore. It is important to keep imaging protocol within an acceptable acquisition duration and yet with high resolution as most of the patients will not be able to tolerate the long scan time and motion artefacts may make interpretation challenging. Therefore, it is paramount to find a balance between resolution and scan time in which our vessel wall protocol is devised to complete in a time efficient manner, within 30 minutes.Our protocol includes T2 -weighted, high-resolution 3D time of flight (ToF) MR angiography, diffusion-weighted imaging (DWI), gradient echo imaging (GRE), post contrast 3D T1-weighted turbo spin echo (TSE) with motion-sensitized driven-equilibrium (MSDE) black blood sequence and post contrast 3D T1-weighted volumetric isotropic fast field echo (FFE). Administration of the contrast agent (gadoterate meglumine, Clariscan 0.05 mmol/mL) is done prior to DWI and GRE sequences to ensure sufficient delay time for optimal contrast enhancement to improve tissue characterization, hence can be used to identify markers of VW inflammation, such as neovascularization (1). All the sequences were performed in axial plane to aid comparison.
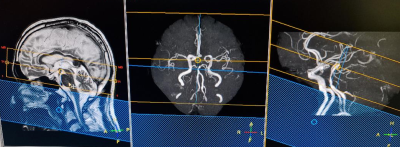
Routine T2-weighted TSE, DWI & GRE sequences of the entire brain are included to rule out presence of abnormality such as old and recent ischemia possibly associated with VW disease (2). 3D TOF MRA sequence is done to assess the arterial lumen and to identify the specific arteries to facilitate the planning of the VW sequence in view of the small field of view. The VW sequence which is the 3D T1-weighted black blood TSE sequence with isotropic voxel size of 0.35mm high spatial resolution can image the small targeted vessels in high definition, coupled with multi-planar capability which permits illustration of the vessels in both short and long axes. The use of MSDE pulse employs flow-sensitive dephasing gradients to suppress blood flow and cerebrospinal fluid (CSF) which plays a major role in the high CNR, thus allowing better visualization of the vessel wall for evaluation [3]. The planning of the 3D T1-weighted TSE is in a transverse oblique angulation so that most anterior circulation arteries can be seen in one slice (Figure 1). Post contrast T1-weighted FFE allows the visualization of the cortical abnormalities, achieving brain morphometry.
Our VW imaging protocol and parameters are illustrated in the table below (Figure 2).
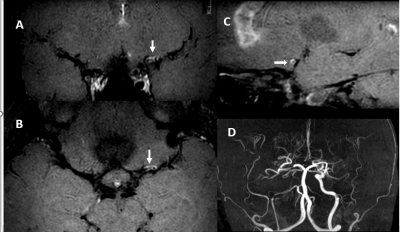
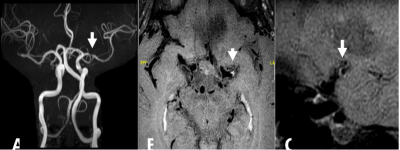
Vessel wall diseases such as atherosclerosis, vasculitis, moya-moya disease and dissection can be shown using the above sequences. These are commonly demonstrated with stenosis on the MRA, wall thickening and sometimes enhancement in inflammatory cases.
Some examples of such cases are shown as below.
A vasculitis case is shown with a stenosis seen in MRA sequence, accompanying with concentric wall thickening (Figure 3).
Another case of an atherosclerosis shown with stenosis on MRA, eccentric wall thickening with wall enhancement (Figure 4).
Conclusion
Our vessel wall imaging protocol is useful in the illustration of many pathologies around the lumen such as intracranial atherosclerosis, vasculitis, intracranial dissection and moya-moya disease within an acceptable imaging duration. While there are practical challenges with regards to common pitfalls on VW imaging, VW imaging still has significant potential in characterizing CNS pathologies.Acknowledgements
No acknowledgement found.References
1. Kang ND, Qiao Y, Wasserman BA. Essential for interpreting Intracranial Vessel Wall MRI Results: State of the Art. Radiology 2021;300:492–505.
2. Lindenholz A, van der Kolk AG, Z:wanenburg JJM, Hendrikse J. The use and pitfalls of intracranial vessel wall imaging: How we do it. Radiology 2018;286(1):12–28.
3. Mandell DM, Mossa-Basha M, Qiao Y, Hess CP, Hui F, Matouk C, Johnson MH, Daemen MJ, Vossough A, Edjlali M, Saloner D, Ansari SA, Wasserman BA, Mikulis DJ. Vessel Wall Imaging Study Group of the American Society of Neuroradiology. Intracranial Vessel Wall MRI: Principles and Expert Consensus Recommendations of the American Society of Neuroradiology. AJNR Am J Neuroradiol. 2017 Feb;38(2):218-229.
4. Havenon AD, Chung L, Park M, Mossa-Basha M. Intracranial vessel wall MRI: a review of current indications and future applications. Neurovascular Imaging 2016; 2:10.
Figures