5407
Cardiovascular magnetic resonance in the evaluation of congenitally corrected transposition of the great arteries1Department of Radiology, Groote Schuur Hospital, Cape Town, South Africa, 2Cape Universities Body Imaging Centre, University of Cape Town, Cape Town, South Africa, 3Department of Radiation Medicine, University of Cape Town and Groote Schuur Hospital, Cape Town, South Africa, 4Division of Cardiology, Department of Medicine, University of Cape Town, Cape Town, South Africa, 5Cape Heart Institute, Faculty of Health Sciences, University of Cape Town, Cape Town, South Africa
Synopsis
Congenitally corrected transposition of the great arteries (ccTGA), is a rare cardiac anomaly (occurring in less than 1% of all congenital heart diseases) characterised by atrio-ventricular and ventricular-arterial discordance. We report on a 13-year-old female with situs inversus totalis, ccTGA, peri-membranous VSD, and sub-PS presenting with worsening fatigue on physical exertion, excessive sweating, and intermittent palpitations not associated with physical activity. Echocardiography was used in diagnosis. CMR revealed mild systolic impairment (ejection fraction, EF 55%) of the systemic ventricle (morphologic RV), a perimembranous VSD, flattening of the interventricular septum in systole and diastole, indicative of pressure and volume overload, respectively.
Background
Congenitally corrected transposition of the great arteries (ccTGA), commonly known as levo or L-looped transposition of the great arteries (L-TGA), is an uncommon cardiac anomaly with atrio-ventricular (AV) and ventriculo-arterial (VA) discordance, occurring in less than 1% of all congenital heart diseases1,2. Associated anomalies are present in more than 90% of patients with ccTGA and include patent ductus arteriosus (PDA), secundum atrial septal defect (ASD), large inlet ventricular septal defect (VSD), and pulmonary atresia. VSD, pulmonary stenosis (PS), left AV valve regurgitation, and/or complete heart block are commonly seen in up to 80% of all cases. ccTGA is rarely associated with situs inversus totalis. Elevated pressures in cardiac chambers can cause ventricular dysfunction and arrhythmias if untreated3. Cardiovascular magnetic resonance (CMR) is important in assessing morphology of the heart, the complex anatomy, and function in patients with ccTGA.Case report
We report on a 13-year-old female with situs inversus totalis, ccTGA, peri-membranous VSD, and sub-PS, who has not had any intervention to-date. She has been asymptomatic until recently when she presented with fatigue on physical exertion, excessive sweating, and intermittent palpitations not associated with physical activity. On clinical examination, she was acyanotic, without any dysmorphic features. There was no cardiomegaly. On auscultation, she was noted to have a loud A2 and a grade 3 ejection systolic murmur at the right upper sternal border in keeping with right outflow tract obstruction. Echocardiography confirmed ccTGA with a dextrocardia, perimembranous VSD, and sub-PS with peak gradient up to 73mmHg. Pulmonary arteries were normal in caliber with no branch or distal stenosis. There were no valvular abnormalities. Cardiac function was normal. CMR was requested to assess right ventricular (RV) and LV size and function, the nature of the PS, pulmonary valve (PV) morphology, and anatomy of the branch pulmonary arteries.Methods
Patient was scanned on a 1.5 Tesla Siemens Magnetom Aera (Erlangen, Germany) MRI scanner using a standard CMR protocol.Results
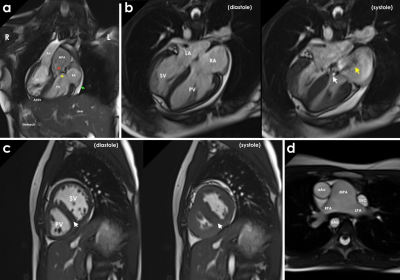
CMR revealed AV and VA discordance in keeping with ccTGA with dextrocardia and situs inversus totalis (Fig. 1a). The systemic ventricle (morphologic RV) had mild systolic impairment (ejection fraction [EF] 55%), normal volumes (end-diastolic volume [EDV] 107ml, EDV indexed to body surface area [BSA] 78ml/m2, Z-score 0.07, end-diastolic dimension [EDD] 37mm) and normal global wall motion with segmental wall thicknesses varying between 5-7mm. Systemic ventricular mass index was within normal range (33g/m2) and with an unobstructed outflow tract. The interventricular septum had a perimembranous VSD with a jet directed to the posterior leaflet of the pulmonic AV valve (Fig. 1b). There was flattening of the septum in systole and diastole, indicative of pressure and volume overload, respectively (Fig. 1c). The pulmonic ventricle (morphologic LV) had normal systolic function (EF 76%), normal volumes (EDV 81ml, EDV indexed to BSA 59ml/m2, Z-score -3.23, EDD 38mm) with a hypertrophied wall (7mm). There were no regional wall motion abnormalities and the outflow tract was normal. Both atria had normal morphology and size (with an area of 19cm2) and there was no interatrial connection. Mild regurgitation was noted through the systemic AV valve (morphologic tricuspid valve) and severe regurgitation through the pulmonic AV valve (morphologic mitral valve) (Fig. 1b). There was no regurgitation or stenosis of the aortic valve and the aortic caliber was within normal limits. The PV was stenosed with leaflet fusion and an area of 1.4cm2. There was subpulmonic flow acceleration due to the systolic anterior motion of the valve leaflet and severe PV stenosis and regurgitation present (Fig. 1a). The main pulmonary artery (MPA) was dilated (38mm), however both right and left pulmonary arteries were within normal limits (Fig. 1d). The inferior vena cava (IVC) was dilated (24mm). A pericardial effusion (7mm) was noted, without any pericardial masses, and the pericardium was of normal thickness (Fig. 1a).Teaching Points
1. CMR provided high-quality imaging that was able to confirm and expand on findings seen on echocardiography.2. CMR provided accurate haemodynamic and valvular integrity measurements.
3. Assessment of the course and morphology of large vessels provides a comprehensive overview of the anatomy.
Conclusion
CMR demonstrated the pathologies and adaptions associated with ccTGA. Furthermore, CMR played a pivotal role in determining whether this patient would benefit from cardiac resynchronization therapy or whether surgical intervention is needed.Acknowledgements
No acknowledgement found.References
1. Munaf, M., Farooqui, S., Kazmi, S. K., & Ul-Haque, I. (2020). Congenitally corrected transposition of great arteries with dextrocardia, patent ductus arteriosus, atrial septal defects and ventricular septal defects in a 15-year-old marfanoid habitus patient: A case study. Cureus, 12(6), e8937.
2. Sekar, B., Marsden, H., & Payne, M. N. (2017). Congenitally corrected transposition of great arteries. Case Reports. British Medical Journal, 2017, bcr-2017.
3. Chinawa, J. (2021). Congenital corrected transposition of the great artery (ccTGA): A complex cardiac anomaly: Challenges in management in a resource poor country: A review article. Journal of Clinical and Experimental Cardiology, 12(7),1-8.
Figures