5399
Improving Visualization of Cervix in MRI with Sterile Surgical Lubricant
Stephan Jordan1, Rebecca Rakow-Penner1, Alex Schlein1, Elin Lundstrom1,2,3, Summer Batasin1, and Stephane Loubrie4
1Radiology, UCSD, La Jolla, CA, United States, 2Department of Surgical Sciences, Uppsala University, Uppsala, Sweden, 3Center for Medical Imaging, Uppsala University Hospital, Uppsala, Sweden, 4UCSD, La Jolla, CA, United States
1Radiology, UCSD, La Jolla, CA, United States, 2Department of Surgical Sciences, Uppsala University, Uppsala, Sweden, 3Center for Medical Imaging, Uppsala University Hospital, Uppsala, Sweden, 4UCSD, La Jolla, CA, United States
Synopsis
MRI is recommended by FIGO for staging of cervical cancer, and thus appropriate visualization of the vaginal vault and cervix is important for accurate staging. MRI has superior soft tissue contrast compared to other imaging modalities. However, when the vaginal vault is decompressed or the prescription angle is off axis, the utility of MRI becomes limited in evaluating cervical cancer. In this abstract, we explore the use of sterile water-based surgical lubricant as a tool to improve visualization of the cervix and associated structures during MRI.
Background
MRI reliably detects abnormalities in the uterus and cervix when a correct prescription of the oblique tilt angle is applied. Positioning of the uterus and cervix varies by patient, making prescription of the tilt angle variable and dependent on the experience of the MRI technologist. Improper prescription of the tilt angle can limit the utility of MRI and visualization of the area of interest for the radiologist. Proper education on the self-administration procedure of the lubricant and its benefits for both MR technologist and radiologist can improve overall quality of cervical imaging.Method
Prior to the exam, approximately 60 mL of sterile surgical lubricant is placed in a non-locking syringe and Yankauer suction catheter is cut approximately 4 cm from its proximal end and placed snugly over the catheter tip. The syringe is stored upright with the catheter facing upward to allow air to escape prior to administration.Patients are asked to insert the lubricant themselves and are educated on the purpose of its administration before the MR technologist leaves the room for privacy. The surgical lubricant tube, gloves, flexible Yankauer, and syringe are given to the patient and an absorbent pad is placed on the MR table underneath the patient. The lubricant delivery takes less than three minutes and is generally well tolerated.
Teaching Point
The use of surgical lubricant during cervical MRI does not add significant time to the MR procedure and improves visualization of the cervical anatomy, particularly in post-menopausal patients and those patients with a partial hysterectomy. The use of lubricant benefits both MR technologists and radiologists in the prescription and analysis of cervical MR images.Summary/Conclusion
Distention of the vaginal cavity with sterile surgical lubricant improves MRI evaluation of the female pelvis, as well as aids diagnosis and staging of cervical cancer. With lubricant distention, the vaginal fornices, as well as the cervix, are clearly defined (particularly on T1 and T2 imaging), which optimizes the ability for MR technologists to prescribe the correct oblique tilt angle (as demonstrated in figures 1 and 2). Surgical lubricant may also be replaced with ultrasound gel (as demonstrated in figure 3), as both provide adequate distention of the vaginal canal.Acknowledgements
No acknowledgement found.References
Brown, Michèle & Mattrey, Robert & Stamato, Stephan & Sirlin, Claude. (2005). MRI of the female pelvis using vaginal gel. AJR Am J Roentgenol. AJR. American journal of roentgenology. 185. 1221-7. 10.2214/AJR.04.1660.Figures
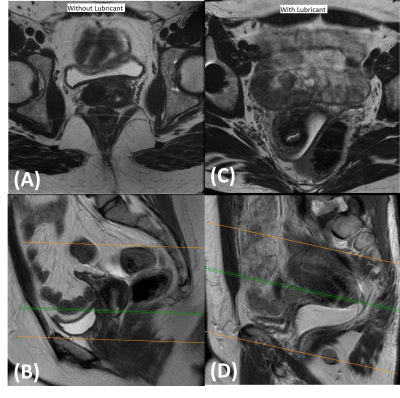
Figure 1 – Acquisitions on two different
healthy patients. T2 acquisitions without lubricant are shown for patient 1 in
the (A) axial and (B) sagittal planes. T2 acquisitions with lubricant are
shown for patient 2 in the (C) axial and (D) sagittal planes.
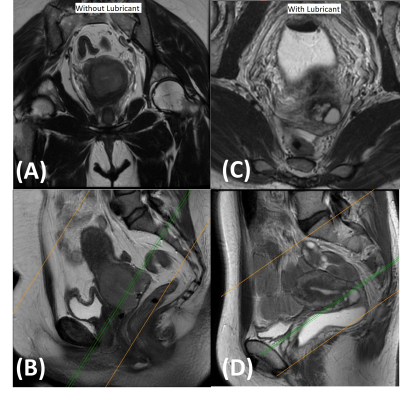
Figure 2 – Acquisitions on two different
cervical cancer patients. T2 acquisitions without lubricant are shown for
patient 1 in the (A) axial and (B) sagittal planes. T2 acquisitions with
lubricant are shown for patient 2 in the (C) axial and (D) sagittal planes.
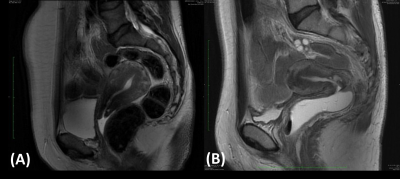
Figure 3 – Sagittal T2 acquisitions on two different
cervical cancer patients (A) with ultrasound gel and (B) with surgical
lubricant.
DOI: https://doi.org/10.58530/2023/5399