5394
Technologist Assessment of a Realtime Motion Monitoring System for fMRI Exams1Radiology, Boston Children's Hospital, Boston, MA, United States, 2Computational Radiology Laboratory, Boston Children's Hospital, Boston, MA, United States, 3Neurology, Boston Children's Hospital, Boston, MA, United States
Synopsis
Visit any magnetic resonance imaging (MRI) facility, and all will agree that patient motion is an ongoing matter. This holds particularly true for pediatric facilities performing functional MRI (fMRI) exams. During fMRI exams, motion artifacts are subtle and contribute to data corruption which is not discovered until the data is analyzed. To enable the technologist to intervene when motion occurs, a real-time motion monitoring system “Slice Localization Integrated MRI Monitoring” (SLIMM) was established to detect motion and reduce the amount of scan time necessary while simultaneously increasing the quality of data collected.
Background
During pediatric brain exams, resting state and task-based fMRI sequences can have lengthy durations of up to 16 minutes each making it difficult for patients to remain motionless. Motion artifacts can be caused by physical and physiological motion. Often children experience anxiety and claustrophobia due to the confining head coil and loud noises, which in turn triggers them to be uncooperative and move. Physiological motion artifacts can originate from the patient's breathing or cardiac cycle (1) causing subtle disturbances in the image quality. It has been estimated in the United States, motion artifacts cost a facility approximately $115,000 per a scanner yearly (2). Motion during a BOLD 2D EPI acquisition results in corrupted BOLD signal data, resulting in a non-diagnostic exam, and the possibility of patient requiring another exam with pharmaceutical interventions. One study concluded the cost of an MRI with anesthesia was 9.56 times higher than that of a conscious patient (3). Due to the low-resolution appearance of BOLD 2D EPI sequences during imaging, the technologist isn’t aware of motion artifacts until the data has been analyzed. At this point, the patient is no longer at the facility and the opportunity to collect crucial data has passed. At our pediatric facility, approximately 50% of the fMRI data collected is discarded due to motion artifacts. To help alleviate the amount of corrupt data collected, scientists in our lab created a novel motion monitoring system called SLIMM (Slice Localization Integrated MRI Monitoring).Method
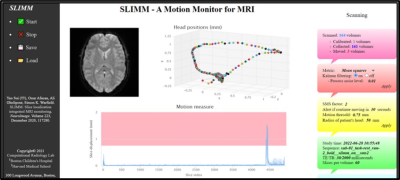
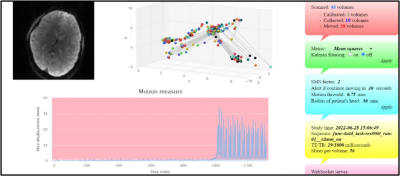
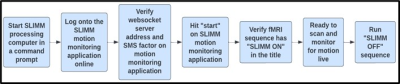
SLIMM motion monitoring allows for the technologist to view the patient’s head motion in real time and as each volume is acquired, the motion data is recorded. The participant’s head motion is displayed in multiple fashions such as the DICOM viewer, a motion plot, and a graph that measures slice displacement (Fig. 1). If there is a large amount of motion (greater than 1mm), the slice displacement graph will turn pink alerting the technologist and allowing intervention. In Figure 1, volunteer A was scanned with the SLIMM application collecting and reporting motion data. The volunteer moved their head from left to right and back to center resulting in three motion corrupt volumes being recorded. The motion measure display turned pink signaling to the technologist the motion artifact is greater than 1mm and communication with the volunteer should be made. Volunteer B, displayed in Figure 2, moved during 38 of the 48 volumes collected which signals to the technologist to communicate with the volunteer. To collect motion data with SLIMM, the technologist needs to follow the following workflow displayed in Figure 3. In a command prompt window, the technologist will start the SLIMM processing computer. Next the technologist logs into the SLIMM application on a computer at the scanner control as displayed in Figures 1 and 2. Each fMRI sequence chosen must have the phrase “SLIMM ON” in the title to alert the SLIMM monitor to start recording. When the sequence is complete, SLIMM is alerted to stop recording by running a 10 second “SLIMM OFF'' sequence. During post-processing, the motion data collected by SLIMM will help scientists remove motion corrupt volumes. Data was collected from 10 volunteers, ranging between the age of 22 to 41 with no known neurological diagnoses, who all received the institution's standard clinical fMRI sequences. Each volunteer was consented under an appropriate IRB from our institution and scanned on a Siemens 3T MR scanner (MAGNETOM Prisma, Siemens, Erlangen, Germany). Each participant was asked to both hold still and move for acquisitions to test the SLIMM application.Results
Each volunteer’s motion (either deliberate physical or uncontrollable physiological) was recorded and displayed. We can confirm this by reviewing the motion measures on the SLIMM application and the translational motion data collected. When the motion artifact was larger than 1mm, the motion measure display turned pink, alerting the technologist to stop the sequence and check on the volunteer. This facilitates time savings by not continuing to collect corrupt data.Conclusion
In all 10 volunteers we retrospectively analyzed the data and confirmed that SLIMM was able to detect motions larger than 1mm in all volunteers in real-time. Motion monitoring is likely to be highly beneficial for other types of sequences used in MRI, such as T1w MPRAGE and T2w FSE. If technologists can intervene early during an image acquisition, the result could be shorter exam durations, less repeated exams with costly pharmaceutical interventions, and a higher quality of data collected, resulting in a better patient outcome. Improvements to simplify the setup and utilization of SLIMM, such as eliminating the start and stop functions, would be beneficial for the technologists’ workflow. With growing demands to acquire diagnostic data while shortening exam times and avoiding pharmaceutical interventions, SLIMM is a novel tool which could support these goals and enable a higher quality of data to be collected.Acknowledgements
This research was supported in part by the following grants: NIH-5R01EB019483 and NIH-S10OD025111.References
1. Sui Y, Afacan O, Gholipour A, Warfield SK. SLIMM: Slice localization integrated MRI monitoring. Neuroimage. 2020 Dec;223:117280. doi: 10.1016/j.neuroimage.2020.117280. Epub 2020 Aug 24. PMID: 32853815; PMCID: PMC7735257.
2. Andre JB, Bresnahan BW, Mossa-Basha M, Hoff MN, Patrick Smith C, Anzai Y, Cohen WA, 2015. Toward quantifying the prevalence, severity, and cost associated with patient motion during clinical MR examinations. J. Am. Coll. Radiol 12 (7), 689–695.
3. Vanderby SA, Babyn PS, Carter MW, et al. Effect of Anesthesia and Sedation on Pediatric MR Imaging Patient Flow. Radiology. 2010; 256(1):229-237.doi.org/10.1148/radiol.10091124