5385
Current State and Future Directions of AI Enhanced Radiology Practice for the Development of Screening and Diagnostic Tools
Sam Hashemi1, Saqib Basar1, Ahmed Gouda1, Thanh-Duc Nyugen1, Yosef Chodakiewitz2, Sean London2, and Rajpaul Attariwala1
1Voxelwise Imaging Technology Inc, Vancouver, BC, Canada, 2Prenuvo Inc, Vancouver, BC, Canada
1Voxelwise Imaging Technology Inc, Vancouver, BC, Canada, 2Prenuvo Inc, Vancouver, BC, Canada
Synopsis
Keywords: Machine Learning/Artificial Intelligence, Machine Learning/Artificial Intelligence
The purpose of this educational exhibit is to highlight the importance of the bilateral and evolving relationship between radiologists and Artificial Intelligence experts, and how the coming together of these two fields is ushering in the AI revolution in Radiology and Radiomics. AI methods and tools are helping radiologists perform big data analytics to enhance diagnostic knowledge and capabilities. There is a need for radiologists and AI engineers to collaborate and define the future direction of AI enhanced Radiology practice.Introduction:
In this educational exhibit we explore the relationship between radiologists and the Artificial Intelligence (AI) community, as both the fields of expertise come together to lay the foundation of the next phase of AI enhanced Radiology practice. The learning objectives of this educational exhibit are:1. Understanding the roles and relationship between AI developers and Radiologists, how this relationship came to be and its evolution. The expectations around this relationship and the co-development of AI enhanced Radiology practice.
2. The misperceptions and limitations around the use of AI tools for Radiology, the challenges they face and the monumental task of regulation of this novel technology.
Introduction to Artificial Intelligence models in Radiology:
Artificial Intelligence has had an explosive growth in the last decade, and is defined as the study of agents that can perceive their environment and consequently take actions to achieve their target objectives. AI models are designed to learn from patterns in data and make predictions based on these patterns.1 One of the advantages of using AI models lies in their ability to perform 3D volumetric/voxel wise analysis as compared to the relatively more limited 2D measurements/view that radiologists traditionally rely upon. This 3D capability can be harnessed to simulate the way radiologists view a study in their mind. AI has the benefit of eliminating cognitive and subjective biases2 that typically affects radiologists wherein their skillset is built upon their teaching and experiences. The successful deployment of this technology in the clinic would allow radiologists to do real time assessment of images with AI assistance to enhance the speed, precision and reproducibility of the diagnostic capabilities, thereby making their workflow more efficient. Radiologists will have access to information such as population analysis built into their platform to inform their diagnosis.3Current use of AI in Medicine and Radiology: Real-world lessons from our collaborative AI-enhanced radiology practice
There exists several opportunities for AI to assist physicians in optimizing their work flow. In addition to radiological image analysis, AI tools are being used to analyze histopathological images and are employed in whole body screening programs to deploy novel methods of disease and cancer screening. The AI-Radiology synergy has allowed physicians access to 3D volumetric information about the size and shape of various organs in the body, such as accurately predicting the volume of the prostate and its zones as well as detection and quantification of over one hundred sixty regions of interest in the body. This information will advance our understanding of human physiology and open doors for designing preventive and precision medicine protocols to promote healthy and graceful aging in humans. These areas highlight some of the current applications of AI in Medicine, however, we have not even scratched the surface of the possibilities that this technology can provide physicians.Relationship between Radiology and AI:
Understanding how these technologies are developed would help us understand the relationship between radiologists and AI developers. Radiologists and clinicians need to guide the development of AI tools that are relevant and its outcomes positively impact the patient management systems. Practice of creativity, collaboration and education between these communities would lead to an AI-clinician synergy. An understanding of the limits and capabilities of this technology and mitigation of false perceptions around the use of AI in medicine would improve its widespread adoption.Limitations, regulation and future directions of AI enhanced Radiology:
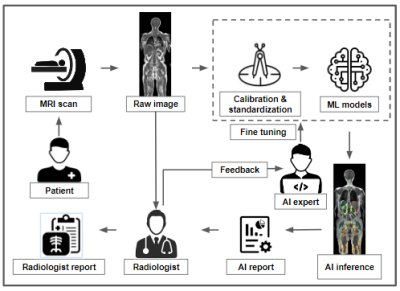
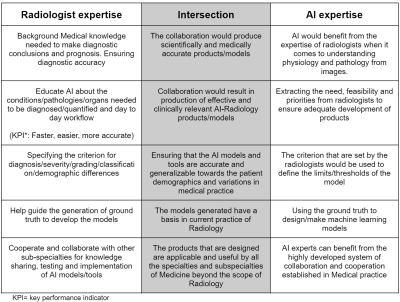
Contrary to popular belief AI is not the magic solution that would eliminate the need for human radiologists. In contrast it is a tool and the usage of this tool will determine how radiologists practice their craft. There are limitations to the current AI technology. The AI experts are limited by the inquiry posed by the radiologists, they can only help with the current workflow practices. There is often a high degree of false prediction due to unexpected factors, such as noise, artifacts and misidentification. Since the technology is evolving it needs large amounts of unbiased and representative samples to train the models to establish high quality reference standards that are reliable, robust and generalizable. The generalizability needs to take into account the different populations and equipment. There needs to be continuous feedback between the radiologists and the AI experts to inform the development of tools. A simplified model of the relationship between the specialists is given in figure 1 and table 1 highlights the intersection of radiologists and AI experts. The models need to be optimized, have minimal overfitting, have clinical utility and strong performance indicators. The AI tools need to be proven to be better than the current and conventional statistical and clinical methods.4 They should be designed to be shareable and transparent. There needs to be adequate frameworks to help regulate this technology such as FDA approval for example and avoid its misuse by rogue actors.Conclusion:
The relationship between radiologists and AI experts needs to be cultivated to develop clinically relevant AI tools that inform the practice of radiologists and physicians. These tools need to be validated on large heterogeneous populations, and have standardized evaluation and regulation criteria. They should be prospective in its design and implementation to make them more robust, unbiased and generalizable to the global patient population. We believe that an AI-clinician synergy is the future direction in the practice of precision medicine.Acknowledgements
We would like to thank the MRI Technologists, Patient Care, and Backend teams for their contributions in the data contribution.References
- Bhattacharya I, Khandwala YS, Vesal S, et al. A review of artificial intelligence in prostate cancer detection on imaging. Ther Adv Urol. 2022;14:17562872221128791. Published 2022 Oct 10. doi:10.1177/17562872221128791
- Bruno MA. 256 Shades of gray: uncertainty and diagnostic error in radiology. Diagnosis (Berl). 2017;4(3):149-157. doi:10.1515/dx-2017-0006
- Wismüller A, DSouza AM, Abidin AZ, et al. Early-stage COVID-19 pandemic observations on pulmonary embolism using nationwide multi-institutional data harvesting. NPJ Digit Med. 2022;5(1):120. Published 2022 Aug 19. doi:10.1038/s41746-022-00653-2
- Koçak B. Key concepts, common pitfalls, and best practices in artificial intelligence and machine learning: focus on radiomics. Diagn Interv Radiol. 2022;28(5):450-462. doi:10.5152/dir.2022.2112972
DOI: https://doi.org/10.58530/2023/5385