5365
An exploratory study to investigate the effect of light music on whole-heart coronary MRI1MRI, Wuhan asia general hospital, Wuhan,HUBEI, China, 2Philips Healthcare,Beijing, Beijing, China
Synopsis
Keywords: Vessels, Cardiovascular, compressed sensing
Whole-heart coronary magnetic resonance angiography (MRA) is a noninvasive, contrast-free, and radiation-free technique for evaluating the origin, morphology, and stenosis of coronary arteries. Nonetheless, a patient's anxious mood results in a longer scan time or lower imaging quality. Previous research has shown that listening to music can alleviate anxiety in patients with coronary heart disease (CHD). In this study, we found no statistical difference in scanning time and imaging quality with CS acceleration factors (AFs) of 2,4,6 in the music and no-music groups. Music may not be necessary during coronary MRA scanning with the CS technique.Introduction
Coronary artery disease is still the leading cause of morbidity and mortality in the world[1]. A novel noninvasive, contrast-free, and radiation-free technique for evaluating the origin, morphology, and lumen stenosis of coronary arteries is whole-heart coronary magnetic resonance angiography (MRA) with compressed sensing (CS). However, the loud noise and relatively enclosed environment of the scanner room may cause anxiety in patients, resulting in a negative impact on heart rate and breathing state, which may lengthen the scanning time or degrade image quality. Previous research has shown that listening to music can reduce patient tension and anxiety, as well as stabilize the patient's respiratory rate and heart rate[2], potentially shortening the scanning time and improving image quality. The goal of this research was to see if light music could improve image quality and scanning time in whole-heart coronary MRA with different compressed sensing acceleration factors.Materials and methods
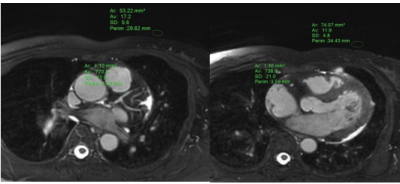
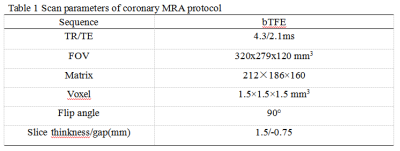
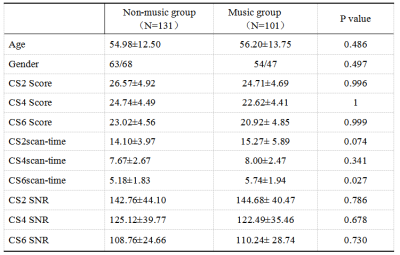
The institutional IRB approved this study. This study enrolled 232 patients to undergo coronary MRA on a clinical 1.5T MR scanner (Ambition, Philips Healthcare, the Netherlands) with a 32-channel body coil, divided into music groups (101 patients, mean age: 5614 years, 54males, 47 females) and non-music groups (131 patients, mean age: 5513 years, 63males, 68 females). The MR protocols with CS AFs of 2,4,6 were based on a navigator-gated steady-state free precession sequence triggered by a free-breathing electrocardiogram[3]. In our study, two groups with the same AFs and parameters were set up, and the scan parameters are shown in Table 1. In case the results were influenced by the patients' state during the long acquisition, a total of three examinations were performed in random order for each patient (about 30min). For qualitative image analysis, we used a four-point subjective scale: 4, excellent (vessel well depicted with sharply defined borders); 3, good (vessel adequately visualized with only mildly blurred borders); 2, fair (coronary vessel visible, but low confidence in the diagnosis due to moderately blurred borders); and 1, poor (coronary vessel barely seen or obscured by noise)[4]. SNR was calculated by manually drawing ROIs on coronary and background images (Figure 1). During scanning, the real scanning time data of CS AFs 2,4,6 were recorded. The Chi square test was used to compare the gender differences between the two groups; the superiority trail was used to calculate the image quality score; and the t test was used to calculate the scanning time and signal-to-noise ratio.Results
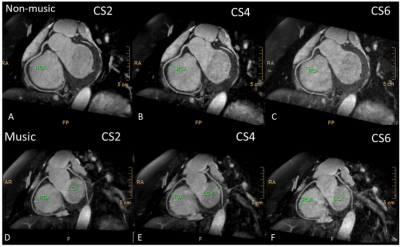
Figure 2 depicts representative images of the RCA and LCX with various AFs. Table 2 shows the differences in CS2, 4, and 6 image quality scores, SNR, and scanning time between the two groups. Although there was no significant difference in image quality scores of CS2, 4, and 6 between two groups [CS2: (24.71 4.69) vs (26.57 4.92), P = 0.996], [CS4: (22.62 4.41) vs (24.74 4.49), P = 1], [CS6: (20.92 4.85) vs (23.02 4.56), P = 0.999], the image quality score of the non-music group was higher. The scanning time of CS2, 4, and 6 in the music group was longer than that of the non-music group [CS2: (15.27 5.89) vs (14.10 3.97), P = 0.074], [CS4: (8.00 2.47) vs (7.67 2.67), P = 0.341], and there was no statistical significance (P > 0.05). The measured SNR of two groups did not differ significantly (P > 0.05): [CS2: (144.68 40.47) vs (142.76 44.10), P = 0.786], [CS4: (122.49 35.46) vs (125.12 39.77), P = 0.416], and [CS6: (110.24 28.74) vs (108.76 24.66), P = 0.730].Discussion
According to our large sample size study, listening to music does not improve image quality or signal-to-noise ratio, nor does it shorten scanning time in whole-heart coronary MRA, which was unexpected. There could be two reasons for this: 1. The effect of music on human heart rate and respiration was insignificant enough to have an effect on the final scanning results. 2, Everyone in our music group listened to the same light music, and different musical styles may have different effects on heart rate and respiration. More research is needed to assess the effect of truly patient-preferred music, as well as the effect of music on patients with varying characteristics.Conclusions
This study shows that listening to music while scanning does not improve image quality or signal-to-noise ratio, nor does it shorten scanning time in whole-heart coronary MRA with different acceleration factors. Music may not be required during coronary MRA scanning.Acknowledgements
On this occasion there is no one we wish to acknowledgeReferences
1. Music for stress and anxiety reduction in coronary heart disease patients. Cochrane Database of Systematic Reviews.
2.Masashi Nakamuraa, Tomoyuki Kidoa, Teruhito Kidoa, Kouki Watanabe, et al. Non-contrast compressed sensing whole-heart coronary magnetic resonanceangiography at 3T: A comparison with conventional imaging. European Journal of Radiology 104 (2018) 43–48.2.Bradt, J., Dileo, C., & Potvin, N. (2013).
3.Akcakaya M, Basha TA, Chan RH, et al. Accelerated Isotropic Sub-Millimeter Whole-Heart Coronary MRI: Compressed Sensing Versus Parallel Imaging. Magn Reson Med. 2014
4. Y. Iyama, T. Nakaura, M. Kidoh, et al., Single-Breath-Hold Whole-heart Coronary MRA in Healthy Volunteers at 3.0-T MRI 3 Springerplus, 2014, p. 667.
Figures