5354
Imaging features and differential diagnosis of Zinner's syndrome: what radiologists should know1Guangzhou First People’s Hospital, Guangzhou, China, 2Department of Radiology, Guangzhou First People’s Hospital, Guangzhou, China, 3Philips Healthcare, Guangzhou, China
Synopsis
Keywords: Urogenital, Pelvis
Zinner's syndrome is a rare congenital urogenital abnormality. Since this disease is rare, knowledge about its imaging manifestations by clinical surgeons and radiologists is inadequate. In this study, data of 11 cases of Zinner's syndrome were retrospectively analyzed, and their morphological characteristics on imaging changes were investigated, aiming to improve the knowledge and differential diagnosis of this disease. The relevant images of Zinner's syndrome show characteristic manifestations, so the seminal vesicle cysts and isolateral kidney development must be carefully observed. Comprehensive judgement should be made according to urogenital mutation or deformity and systemic development situation.Introdution
Zinner's syndrome is a rare congenital urogenital abnormality and mainly includes unilateral renal agenesis or renal hypoplasia complicated with isolateral seminal vesicle cyst and ejaculatory duct obstruction [1-4]. Clinical statistics show the incidence of Zinner's syndrome is only 2.14/100000 [5]. Since this disease is rare, knowledge about its imaging manifestations by clinical surgeons and radiologists is inadequate. In this study, data of 11 cases of Zinner's syndrome were retrospectively analyzed, aiming to improve the knowledge and differential diagnosis of this disease.Materials and methods
The data from 11 Zinner's syndrome patients diagnosed clinically and by imaging between June 2010 and December 2021 were collected. All 11 patients were males aged 22 to 68 years. Their clinical symptoms include hemospermia and infertility (4 cases), frequent urination and urinary incontinence (3 cases), dysuria (2 cases), and occasional discovery upon medical examination (2 cases).Six of the 11 patients received magnetic resonance (MR) plain scan plus enhanced scan, 4 cases underwent computed tomography (CT) plain scan plus enhanced scan, 1 case received CT plain scan first and then MR plain scan plus enhanced scan. The major contents of image reading were to determine: (1) the concrete positions of cysts: lower ureter segment - inner bladder walls, prostate, seminal vesicle or verumontanum;(2) shape: regular shape or not, tube-like or circular, round-like, single or frequently-occurring; (3) size: the largest cyst diameter measured on the cross- section;(4) boundary: whether cystwalls were smooth or not; whether mural nodules existed or not; whether focal margins were blur or not;(5) density or signal of contents: compared with the density or signal of intrabladder urine, and whether bleeding occurred or not;(6) changes in adjacent organs and tissues: whether bladders, prostate and rectum were compressed, and the degree of compression.
Results
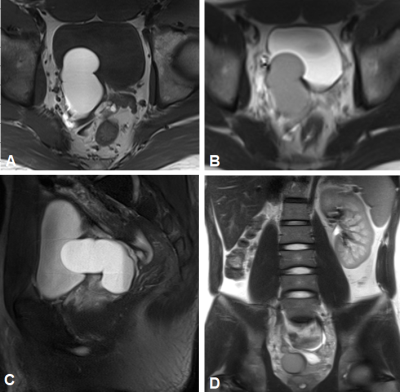
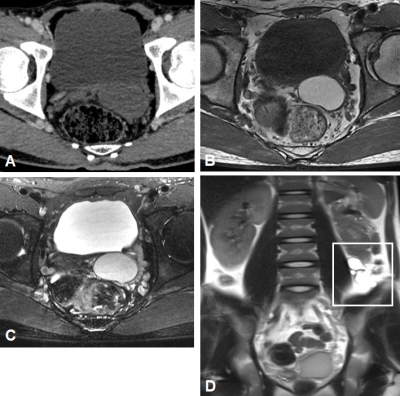
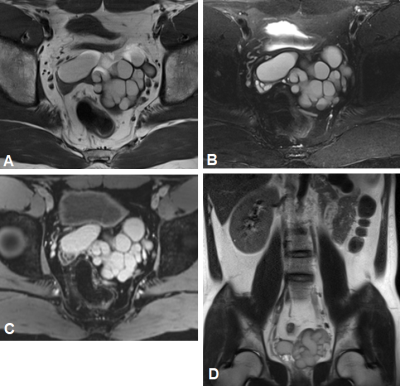
On the abdominal pelvic CT or MR images, 8 cases are manifested as unilateral renal agenesis complicated with isolateral seminal vesicle cyst (6 cases on the right, 2 cases on the left); 2 cases as left renal agenesis complicated with bilateral seminal vesicle dysplasia; 1 case as left renal dysplasia complicated with left seminal vesicle cyst. Nine cases have single-shot cysts, which are ovate-shaped with the largest diameter of 3.8-6.5 cm (6.2±2.3 cm); 2 cases have significant cystic dilation. On the CT images, the cysts are manifested as hypointensity (2 cases, simple cysts), or hyperintensity (3 cases, complicated cysts) higher than that of intrabladder urine. The range of CT values is 3-52 HU (median of 36 HU). The inner part of enhanced scans is not enhanced. MR images show hypointensity (2 cases, pure cysts) or hyperintensity (5 cases, complicated cysts) on T1WI, and hyperintensity on T2WI in all cases, with liquid-liquid planes in 3 cases. Seven patients were compressed obviously at unilateral bladder posterior walls, 2 patients were slightly compressed at unilateral prostate, and 6 cases were compressed and changed at rectum anterior walls.Discussion
The major cystic lesions of prostate-seminal vesicle are seminal vesicle cysts, Mullerian duct cysts, and ejaculatory duct cysts. According to the position, shape and compression way of cysts, seminal vesicle cysts can be easily differentiated from Mullerian duct cysts and ejaculatory duct cysts. The seminal vesicle cyst is located at one side or both sides of the seminal vesicle and is separated by prostate capsules from the prostate and surrounded by seminal ducts. It is either single or multiple, and the large cysts can compress the posterior bladderic walls [6]. The Mullerian duct cyst is located at the verumontanum between the middle of the prostate and the bilateral seminal vesicle, and results from incomplete degeneration of the Mullerian duct formed inside the prostate. The Mullerian duct cyst is single and not connected with the seminal duct. It protrudes upwards the bladder, and its lower part is sharp and extends to the prostate. The sagittal plane or coronary plane is typically inverted and drop-like [7]. The ejaculatory duct cyst is located at the verumontanum in the posterior urethra prostate and is often single and unilateral. It is induced by ejaculatory duct dilatation. On the cross-section, it points from the outer posterior to the inner anterior. On the coronary plane, it extends from the outer superior to the lower inner part. It often does not compress or alter the bladder and rectum.After confirmation as seminal vesicle cyst, the key to differential diagnosis is to differentiate between Zinner's syndrome-related or simple seminal vesicle cyst. A Zinner's syndrome seminal vesicle cyst can be regarded as a special seminal vesicle cyst and is further developed from the central nephridium structure (ureteric residues) remaining in the seminal vesicle and is correlated with the maturity and hormone level of the reproductive system [8]. When symptoms appear, it is usually manifested as a large-volume round-like or irregular polycystic tube-like structure, which significantly suppresses the ipsolateral posterior bladder walls. In comparison, simple seminal vesicle cysts only locally expand in the seminal duct and are regularly shaped, which is either round or ovate-like.
Conclusion
The images of Zinner's syndrome show characteristic manifestations, so the seminal vesicle cysts and isolateral kidney development must be carefully observed. Comprehensive judgement should be made according to urogenital mutation or deformity and systemic development situation.Acknowledgements
No acknowledgement found.References
[1] Fuselier HA, Peters DH. Cyst of seminal vesicle with ipsilateral renal agenesis and ectopic ureter: case report[J]. J Urol,1976,116(6):833-835.
[2] Ouden D, Blom JH, Bangma C, et al. Diagnosis and management of seminal vesicle cysts associated with ipsilateral renal agenesis:a pooled analysis of 52 cases[J].Eur Urol ,1998;33(5):433-440.
[3] Cihan A, Cimen S, Secil M, et al. Congenital seminal vesicle cyst accompanying ipsilateral renal agenesis and rudimentary ureter[J]. Int Urol Nephrol,2006,38(1):133-135.
[4] Pace G, Galatioto GP, Gualà L, et al. Ejaculatory duct obstruction caused by a right giant seminal vesicle with an ipsilateral upper urinary tract agenesia: an embryologic malformation[J].Fertil Steril,2008,89(2):390-394.
[5] Pereira BJ, Sousa L, Azinhais P, et al. Zinner's syndrome: an up-to-date review of the literature based on a clinical case[J]. Andrologia,2009,41(5):322-330.
[6] Khanduri S, Katyal G, Sharma H, et al. Unique Association of Multiple Seminal Vesicle Cysts with Contralateral Renal Agenesis: A Rare Variant of Zinner Syndrome[J]. Cureus, 2017,9(7):e1415-e1418.
[7] Tan ZW, Li B, Zhang L, et al. Classifying seminal vesicle cysts in the diagnosis and treatment of Zinner syndrome: A report of six cases and review of available literature[J].Andrologia,2019,52(1):e13397.
[8] Seo IY, Kim HS, Rim JS. Congenital seminal vesicle cyst associated with ipsilateral renal agenesis[J]. Yonsei Med J,2009,31;50(4):560-563.
Figures