5346
Differential lesion volume progression following MR-guided focused ultrasound thalamotomy for Essential Tremor1Radiology and Clinical Neurosciences, Cumming School of Medicine, University of Calgary, Calgary, AB, Canada, 2Hotchkiss Brain Institute, Cumming School of Medicine, University of Calgary, Calgary, AB, Canada, 3University of Calgary, Calgary, AB, Canada, 4Dept of Psychology, St Francis Xavier University, Antigonish, NS, Canada, 5Dept of Surgery, University of Alberta, Edmonton, AB, Canada, 6Dept of Surgery, University of Calgary, Calgary, AB, Canada
Synopsis
Keywords: Neurodegeneration, Focused Ultrasound, Movement disorders; treatment
Following MRgFUS thalamotomy for Essential Tremor, it was observed that lesions in some patients re-enlarged after the 3-month timepoint following surgery, based on T1-weighted MRI. After grouping patients as NonEnlargers and Enlargers based on this observation, we did not observe significant between-group differences in clinical measures of tremor beyond the 3-month timepoint. Patient demographic- and MRgFUS-related factors did not differ between groups. However, patients in the NonEnlarger group demonstrated significantly greater tremor severity prior to and in early timepoints following MRgFUS thalamotomy, suggesting that the relationship between tremor severity and longitudinal lesion progression may be worthy of further investigation.INTRODUCTION
Essential Tremor (ET) is a disabling movement disorder that affects 5% of those over the age of 651,2. For those with severe disabling ET, and for whom pharmaceutical treatment is not effective or tolerated, surgery is a possible option.Magnetic-resonance-guided focused ultrasound (MRgFUS) thalamotomy is an emerging surgical procedure for ET, targeting the thalamic Ventral Intermediate nucleus (VIM). Following MRgFUS thalamotomy, lesions are known to dramatically decrease within 3 months after surgery1,3,4. However, the few MRI studies following lesion presentation until 1-year post-surgery have reported either mixed lesion visibility or assumptions of lesion resolution4-6.
Several studies have reported that larger lesions observed within the first 3 months following MRgFUS thalamotomy were associated with better clinical tremor outcomes1,4,5,7. However, few studies describe relationships between MRgFUS lesion volume and clinical measures until the 1-year post-surgical timepoint5, and none have explored these relationships between the 3-month and 1-year period or beyond.
Introductory Observation:
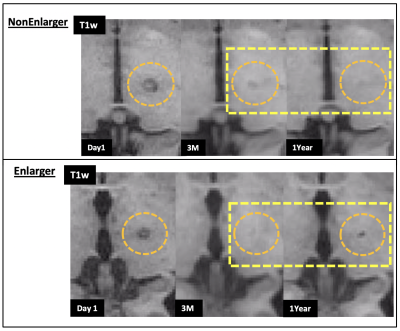
During routine MRI inspection of our patients, we observed that lesions in some patients re-enlarged after 3 months (see Figure 1). To our knowledge, this phenomenon has not been explicitly investigated. Therefore, the aims of the present study were to (1) describe differential longitudinal lesion volume evolution on T1-weighted MRI, (2) examine potential patient and treatment factors related to lesion change, and (3) investigate whether relationships exist between late lesion volume change and clinical measures of tremor.
METHODS
Participants:18 Essential Tremor patients (73.1±7.7y, 17M 1F) from a pool of 28 patients who underwent surgery in our centre between May 2017 and June 2020. Exclusion criteria: previous neurosurgeries, poor MRI quality, conflicting movement disorder diagnoses. A subset of these patients with 2-year clinical data (n=13, 73.0±9.2y, 12M 1F) was studied in an additional analysis.
MRI:
MRI data were collected using a 3T Discovery 750 (GE Healthcare) and a 32-channel head coil (Nova Medical). T1-weighted anatomical volumes [3D FSPGR (BRAVO) [TR/TE/TI: 8.156/3.172/650 ms, flip angle=10o, 256x256matrix, 256mm FOV, 188 slices, 1 mm3 voxel]] were used in this analysis. MRIs were obtained PRE surgery, 24 hours post-surgery (Day1), 3 months (3M), and 1 year (1Yr).
Clinical measures:
The Clinical Rating Scale for Tremor8 (CRST) was used to assess tremor severity at PRE surgery, 3M, 1Yr, (and 2 years in a 13-patient subset (2Yr)). Measures considered were the Overall score (parts A, B, C), and subscores 'Hand with Writing' (part B), 'Upper Extremity' (part A), both pertaining to the treated side only. (Higher scores indicate more severe tremor.)
Lesion Volumetry:
Lesion regions-of-interest were manually defined on T1-weighted images using FSLeyes (FSL9). Lesion volumes were analyzed using raw values and Day1-normalized percentages.
Patient Grouping:
Patients were divided into "NonEnlarger" (n=9) and "Enlarger" (n=9) groups, defined by lesion volumetric change between the 3M and 1Yr timepoints. For the subset of patients with 2-year clinical data, there were 5 NonEnlargers and 8 Enlargers.
Between-group Patient Factors:
Age and time between data timepoints were compared between groups, as were surgical focused ultrasound parameters (temperature, thermal dose, # sonications).
Statistics:
Between-group analysis was performed using Mann-Whitney U using the Real Statistics Resource Pack (v7.6, Zaiontz C, www.real-statistics.com). As this was an exploratory study, no corrections made for multiple comparisons.
RESULTS
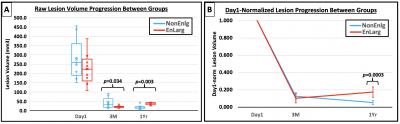
Lesion volumetry:The NonEnlarger group showed greater lesion volumes vs Enlarger group at the 3M timepoint (p=0.034, see Figure 2a). Day1-normalized lesions were remarkably similar between groups between the Day1 and 3M timepoints (see Figure 2b).
Patient/Treatment Factors:
A group difference was observed in duration between Day1 and 3M timepoints (NonEnlargers 105±39.9 days, Enlargers 96±11.2 days, p=0.042). No other between-group differences between timepoints were observed. Furthermore, no age differences were observed between groups, nor were there differences in focused ultrasound treatment parameters.
Clinical Measures:
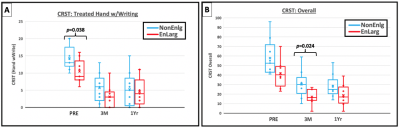
At the PRE timepoint, the CRST subscore of 'Hand with Writing' was greater in the NonEnlarger vs Enlarger group (p=0.038, see Figure 3a). At the 3M timepoint, the overall CRST score was greater in the NonEnlarger vs Enlarger group (p=0.024, see Figure 3b). No other CRST measures were found to differ between groups at any timepoint or between timepoints. Additionally, the 2Yr subset observed no significant between-group differences.
DISCUSSION
We describe the novel finding that lesions re-enlarge in some ET patients after the 3-month timepoint following MRgFUS thalamotomy.The fact that patients with re-enlarging lesions had more severe tremor at baseline and 3-months following surgery suggests that there may be an inherent difference in brain composition in patients with greater tremor. However, the present study did not find any relationships between lesion re-enlargement and clinical outcome at timepoints 12 months or beyond following MRgFUS thalamotomy. That said, this lack of difference in tremor severity may also relate to small sample size and variability within patient groups.
We continue to examine longitudinal MR changes in these patients, utilizing correlations to further investigate relationships between lesion volume and clinical outcome.
CONCLUSIONS
Lesions on T1-weighted MRI may later re-enlarge after FUS thalamotomy, but the presence of this re-enlargement showed no direct relationship with later-stage clinical outcomes. However, lesion re-enlargement appeared more commonly in patients with more severe tremor prior to and early followup to MRgFUS thalamotomy.Acknowledgements
No acknowledgement found.References
1. Wintermark M, Druzgal J, Huss DS, et al. Imaging Findings in MR Imaging-Guided Focused Ultrasound Treatment for Patients with Essential Tremor. Am J Neuroradiol 2014; 35:891-896.
2. Govert F, Becktepe JS, Deuschl G. Current concepts of essential tremor. Revue Neurologique 2016; 172:416-422.
3. Elias WJ, Huss, D, Voss T, et al. A Pilot Study of Focused Ultrasound Thalamotomy for Essential Tremor. N Engl J Med 2013; 369:640-648.
4. Kapadia AN, Elias GJN, Boutet A, et al. Multimodal MRI for MRgFUS in essential tremor: post-treatment radiological markers of clinical outcome. J Neurol Neurosurg Psychiatry 2020; 91:921-927.
5. Harary M, Essayed WI, Valdes PA, McDannold N, Cosgrove GR. Volumetric analysis of magnetic-resonance-guided focused ultrasound thalamotomy lesions. Neurosurg Focus 2018; 44(2):E6.
6. Bond AE, Elias WJ. Predicting lesion size during focused ultrasound thalamotomy: a review of 63 lesions over 3 clinical trials. Neurosurg Focus 2018; 44(2):E5.
7. Keil VC, Borger V, Purrer V, et al. MRI follow-up after magnetic resonance-guided focused ultrasound for non-invasive thalamotomy: the neuroradiologist’s perspective. Neuroradiology 2020; 62:1111-1122.
8. Fahn S, Tolosa E, Marin C. Clinical rating Scale for Tremor. In: Jankovik J and Tolosa E. Parkinson’s Disease and Movement Disorders. Baltimore-Munich: Urban & Scharzenberg, 1988. p. 225-234.
9. Jenkinson M, Beckmann CF, Behrens TE, Woolrich MW, Smith SM. FSL. Neuroimage 2012; 62:782-790.
Figures