5291
Optic nerve thickening on high-resolution MRI predicts early-stage postlaminar optic nerve invasion of retinoblastoma.1Radiology, Amsterdam UMC, Amsterdam, Netherlands, 2Diagnostic and Interventional Radiology and Neuroradiology, University Hospital Essen, Essen, Germany
Synopsis
Keywords: Tumors, Tumor, optic nerve invasion; quantitative; pediatric; prediction; metastases;
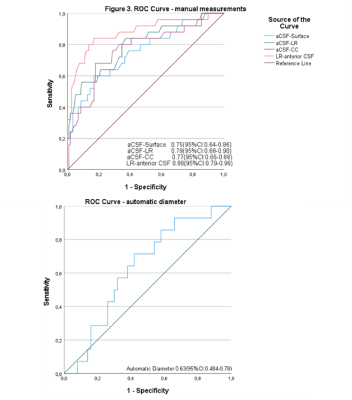
Two radiologists with different levels of experience measured the anterior optic nerve to predict postlaminar optic nerve invasion (PLONI) in retinoblastoma. In addition, quantitative measurements were performed using a deep-learning method 3D U-net. The results showed that measurements performed by the radiologists had an AUC of 0.88 for the detection of PLONI, while the preliminary results of the quantitative approach had an AUC of 0.63. Both methods show promising results to predict early-stage PLONI in retinoblastoma patients.Introduction
Retinoblastoma is a malignant tumor of the retina and is the most frequently occurring eye cancer in children.[1] Retinoblastoma patients have several risk factors for developing metastases, including massive choroidal invasion, scleral invasion, and postlaminar optic nerve invasion (PLONI).[2-4] PLONI is defined as tumor cells extending through the lamina cribrosa sclerae, the barrier between the intra-ocular space and the intradural space, which increases the risk of metastatic tumor spread.[5, 6] Currently, histopathology is the gold standard to evaluate PLONI. However, histopathologic analysis is often not possible since conservative (eye-saving) treatment is increasingly favored. Therefore, magnetic resonance imaging (MRI) plays an important role in retinoblastoma care, especially to determine metastatic risk factors.[7, 8] On MRI, PLONI is generally determined by assessing the presence of gadolinium contrast enhancement in the optic nerve. Even though MRI is helpful to stratify retinoblastoma cases by metastatic risk factors, the diagnostic accuracy for early stage extraocular disease is limited.[9, 10] We hypothesize that the size of the optic nerve assist in predicting tumor extension beyond the lamina cribrosa. In particular, we suspect that thickening of the optic nerve just beyond the level of the sclera can predict tumor invasion, since the lamina cribrosa functions as a natural first barrier for tumor extension. The purpose of this study is to evaluate the diagnostic accuracy of measuring optic nerve size to predict PLONI.Materials and methods
In this multicenter, retrospective, and international case-control study, patients were included from two retinoblastoma referral centers. Patients were categorized in to three groups, PLONI cases (patients with at least one eye with histopathologically proven PLONI), retinoblastoma controls (patients with at least one eye with absence of PLONI), and healthy controls (the healthy contralateral eye of unilateral retinoblastoma patients). Patients were included when 1) patients were diagnosed with retinoblastoma, 2) histopathology was available for at least one of two eyes after primary enucleation, 3) MR images before any treatment were available, including high-resolution 3D T2-weighted images. Patients were excluded when reliable measurement was impossible, i.e. due to motion artefacts.MR image assessment
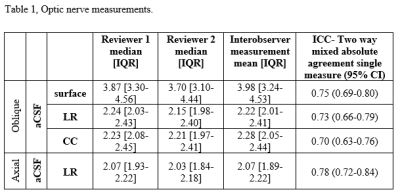
Two readers, respectively with 10 and 1 years of experience, independently measured and scored MR images blinded to clinical and histopathological data. The optic nerve size was measured on the 3D T2-weighted sequence at the level of the most anteriorly located CSF. Original axial 3D T2-weighted images were used to measure the optic nerve width and multiplanar reconstructions were used to measure double oblique width, height, and surface. In addition, the optic nerves were automatically segmented and quantitatively assessed using the method of Elst et al..[11] The interobserver agreement was determined to predict the reliability of measurements and Mann-Withney U test was used for comparison of the mean consensus of three different groups. Diagnostic accuracy of both the manual measurements and automatic measurements were assessed with receiver operating characteristic (ROC) analyses.
Results
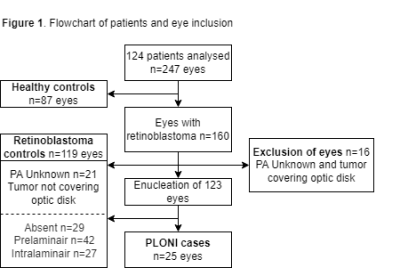
A total of 124 patients (247 eyes) were included. Patients had a median age of 22 months (range, 0-113), 58 (47%) were female. Of the 247 eyes, 160 (65%) were affected by retinoblastoma and 87 (35%) were unaffected and used as healthy controls. Out of 160 eyes that had retinoblastoma, 124 (78%) were enucleated with a median number of 4 days between MRI and enucleation (range, 0-26). Twenty-five eyes (20%) had histopathologically proven PLONI and were classified as PLONI cases. Out of the 37 eyes which were not enucleated, 16 (43%) were covering the optic disk and were excluded from further analysis as they could still have PLONI. A total of 119 eyes were classified as retinoblastoma controls, see Figure 1.Interobserver Agreement
The mean interobserver measurement for the optical nerve width on non-reconstructed axial 3D MRI at the anterior CSF(LR-anterior CSF) was 2.07 [IQR 1.89-2.22]. All the observations and interobserver agreements are shown in Table 1 and showed a good agreement[12].
Comparison of mean consensus for the three groups, PLONI cases, retinoblastoma controls and healthy controls are shown in Figure 2.
ROC Analysis
ROC analysis showed an AUC of 0.88 (95%CI:0.79-0.96) of the axial aCSF width for the prediction of PLONI and slightly lower AUCs for the double oblique measured aCSF width, height and surface area, see Figure 3. The automatically obtained diameters showed an AUC of 0.63 (95%CI:0.48-0.78) for the prediction of PLONI.
Discussion
In comparison to literature to the best of our knowledge we were the first study to measure the optic nerve width to predict PLONI with reasonable results. Similair AUC were found in a study done by Liu et al.[13] with an AUC of 0.87(95%CI:0.78–0.95) while looking at optic nerve enhancement and ADC values of the effected optic nerve. Li et al.[14] used at a more conventional model, which resulted in an comparable AUC of 0.84(95%CI:0.77–0.91).Conclusion
Early stage optic nerve thickening, detectable with modern high-resolution MRI, can predict early stage postlaminar optic nerve invasion, Also, preliminary results of the automatic segmentation of the optic nerve shows promising results when it comes to predicting early stage postlaminar optic nerve invasion and will be explored further.Acknowledgements
We would like to thank all our authors for their contribution.References
1. Moll, A.C., et al., Incidence and survival of retinoblastoma in The Netherlands: a register based study 1862-1995. Br J Ophthalmol, 1997. 81(7): p. 559-62.
2. Finger, P.T., J.W. Harbour, and Z.A. Karcioglu, Risk factors for metastasis in retinoblastoma. Surv Ophthalmol, 2002. 47(1): p. 1-16.
3. Kaliki, S., et al., High-risk retinoblastoma based on international classification of retinoblastoma: analysis of 519 enucleated eyes. Ophthalmology, 2013. 120(5): p. 997-1003.
4. Bosaleh, A., et al., Outcome of children with retinoblastoma and isolated choroidal invasion. Arch Ophthalmol, 2012. 130(6): p. 724-9.
5. Jonas, J.B., et al., Morphometry of the human lamina cribrosa surface. Invest Ophthalmol Vis Sci, 1991. 32(2): p. 401-5.
6. Jonas, J.B., E. Berenshtein, and L. Holbach, Anatomic relationship between lamina cribrosa, intraocular space, and cerebrospinal fluid space. Invest Ophthalmol Vis Sci, 2003. 44(12): p. 5189-95.
7. Mallipatna AC, G.B., ChévesBarrios P, et al., AJCC Cancer Staging Manual, E.S. Amin MB, Greene FL, et al., Editor. 2017, Springer: New York. p. 819-831.
8. de Jong, M.C., et al., Trilateral retinoblastoma: a systematic review and meta-analysis. Lancet Oncol, 2014. 15(10): p. 1157-67.
9. Brisse, H.J., et al., Assessment of early-stage optic nerve invasion in retinoblastoma using high-resolution 1.5 Tesla MRI with surface coils: a multicentre, prospective accuracy study with histopathological correlation. Eur Radiol, 2015. 25(5): p. 1443-52.
10. de Jong, M.C., et al., Diagnostic performance of magnetic resonance imaging and computed tomography for advanced retinoblastoma: a systematic review and meta-analysis. Ophthalmology, 2014. 121(5): p. 1109-18.
11. Elst, S.v., et al., Automatic Segmentation and Quantification of the Optic Nerve on MRI Using 3D U-Net. Submitted, 2022.
12. Koo, T.K. and M.Y. Li, A Guideline of Selecting and Reporting Intraclass Correlation Coefficients for Reliability Research. J Chiropr Med, 2016. 15(2): p. 155-63.
13. Liu, J., et al., Diffusion-Weighted MR Imaging of the Optic Nerve Can Improve the Detection of Post-Laminar Optic Nerve Invasion from Retinoblastoma. J Magn Reson Imaging, 2022.
14. Li, Z., et al., Diagnosis of Postlaminar Optic Nerve Invasion in Retinoblastoma With MRI Features. J Magn Reson Imaging, 2020. 51(4): p. 1045-1052.