5213
Mixed brain perfusion pattern and its association with epilepsy duration: The application of arterial spin labeling in older people with epilepsy1Radiology Department, Huashan Hospital, Shanghai, China, 2Neurology Department, Huashan Hospital, Shanghai, China
Synopsis
Keywords: Epilepsy, Arterial spin labelling
The early identification, evaluation and intervention are important for older people with epilepsy, which calls for techniques of high convenience, repeatability and practicality in clinical application. By applying arterial spin labeling (ASL), we detected perfusion differences between older people with epilepsy and healthy controls on whole-brain voxel-based level, and conducted linear regression between cerebral blood flow (CBF) and duration of epilepsy. Our findings revealed a mixed perfusion pattern for older people with epilepsy, and the significant correlation between CBF and duration of epilepsy. Therefore, ASL has potential value in early diagnosis and evaluation of seizure activity and severity for epilepsy.
Introduction
The population of older people takes up one of the two peaks of epilepsy, which may cause decreased quality of life and higher mortality[1, 2]. The early identification, evaluation and intervention are important for older people with epilepsy, which calls for techniques of high convenience, repeatability and practicality in clinical application. Arterial spin labeling (ASL) has been widely used in neurodegenerative diseases, cerebrovascular diseases and brain tumors[3] for its characteristics of non-invasiveness, non-radiation and easy combination with routine MRI scan sequences[4]. We aimed to investigate the feasibility of applying ASL in older people with epilepsy, by identifying the perfusion pattern of older people with epilepsy on whole-brain voxel-based level, and exploring the impact of duration of epilepsy on the altered cerebral blood flow (CBF).Methods
A total of 80 older people diagnosed with epilepsy according to the International League Against Epilepsy definition[5] and 40 healthy controls were recruited and administrated the high-resolution T1 and ASL magnetic resonance imaging (MRI) scan on a 3.0-T scanner (Discovery MR750W, General Electric, Milwaukee, USA). Clinical seizure variables including age of onset, seizure frequency, duration of epilepsy, and number of anti-seizure medication (ASM) types were collected. The CBF images were directly obtained for data processing. The whole-brain voxel-based analysis was conducted using SPM8 software. Relative CBF of whole-brain in epilepsy and healthy controls was compared by two-sample t-test with age and gender as covariates with Alphasim correction. Mean CBF of brain regions with significant relative CBF differences between the two groups were extracted by DPABI software. The ROI-based correlation between mean CBF and duration of epilepsy was analyzed by linear regression with age of onset, gender, education, seizure frequency, and number of ASM types as covariates using SPSS version 28.0.Results
Compared to healthy controls, two clusters of hypoperfusion and three clusters of hyperperfusion were observed in epilepsy group (P < 0.05, cluster-level, AlphaSim corrected). Older people with epilepsy exhibited decreased CBF in the bilateral middle temporal gyrus and inferior temporal gyrus, and increased CBF in the left supplementary motor area, right fusiform gyrus and left anterior cingulate and paracingulate gyri. After adjustment for age of onset, gender, education, seizure frequency and number of anti-seizure medication types, we found lower CBF in areas of hypoperfusion significantly correlated with longer duration of epilepsy (β=-0.430, P=0.024 for the left middle temporal gyrus and inferior temporal gyrus and β=-0.466, P=0.022 for the right middle temporal gyrus and inferior temporal gyrus).Discussion
For one thing, we found hypoperfusion in the bilateral middle temporal gyrus and inferior temporal gyrus in older people with epilepsy. During the chronic interictal period, cerebral blood flow is typically reduced as the epileptogenic region with recurrent seizure attacks tends to be less active compared with the normal brain tissue[3]. Lower cerebral blood flow represents insufficient delivery of blood oxygen and energy metabolism[6], which may cause nerve dysfunction in the long term. We suppose hypoperfusion as a symbol of clinically inactive stage of epilepsy, and ASL can be a useful imaging technique in detection of epileptogenic lesions and evaluation of seizure activity. For another, we also found hyperperfusion in the left supplementary motor area, right fusiform gyrus and left anterior cingulate and paracingulate gyri. From the perspective of hemodynamics, hyperperfusion was generally seen during the ictal or peri-ictal period of epilepsy as the consequence of pathologic neuronal activity[3], and hyperperfusion may still occur under the circumstance of hypoperfusion due to new-onset epileptic discharges. Moreover, the presence of compensatory hemodynamic changes has been recently reported in epilepsy[7]. It is speculated that the interictal period of epilepsy had the characteristic of preserved pattern of perfusion as a compensatory process, during which cellular and vascular metabolism were overactivated in order to maintain high-level abilities of neurons[8]. We suppose hyperperfusion as a symbol of clinically unstable and overactive stage with preserved blood supply in epilepsy. It indicates the pathophysiological stage of epilepsy progression, and provides additional information on seizure activity, guiding clinical intervention and potential therapeutic evaluation. Additionally, lower cerebral blood flow in brain regions of hypoperfusion significantly correlated with longer duration of epilepsy. Two former researches indicated the significant correlation between longer duration of epilepsy and lower brain glucose metabolism[9, 10], which were in consistency with our study for the close coupling of perfusion and metabolism in the brain. For brain regions with hypoperfusion, cerebral blood flow may be in a diminishing process because of the lasting seizure attacks. It manifests as linear relationship of longer epilepsy duration and less cerebral blood flow, suggesting the value of ASL in evaluating the severity of epilepsy. Hence, recognizing the transition of the perfusion pattern by ASL may be the key point to explore the hemodynamic mechanisms of epilepsy, and guide clinical diagnosis and treatment of identifying seizure activity and stage of epilepsy progression.Conclusion
The presence of the mixed brain perfusion pattern and the significant correlation between cerebral blood flow and duration of epilepsy suggested the potential effectiveness of applying ASL in clinical practice of early diagnosis and evaluation of seizure activity and severity for epilepsy.Acknowledgements
This work was sponsored by the National Natural Science Foundation of China (81971598, 82071456), Shanghai Municipal Science and Technology Major Project (2018SHZDZX01) and ZJ LAB, Shanghai Academic Research Leader Program (21XD1420900), Shanghai Municipal Commission of Health (No.20224Z0002), and “Shuguang Program” supported by Shanghai Education Development Foundation and Shanghai Municipal Education Commission(19SG06).
References
[1] GIUSSANI G, BIANCHI E, BERETTA S, et al. Comorbidities in patients with epilepsy: Frequency, mechanisms and effects on long-term outcome [J]. Epilepsia, 2021, 62(10): 2395-404.[2] SEN A, JETTE N, HUSAIN M, et al. Epilepsy in older people [J]. Lancet, 2020, 395(10225): 735-48.
[3] HALLER S, ZAHARCHUK G, THOMAS D L, et al. Arterial Spin Labeling Perfusion of the Brain: Emerging Clinical Applications [J]. Radiology, 2016, 281(2): 337-56.
[4] ALSOP D C, DETRE J A, GOLAY X, et al. Recommended implementation of arterial spin-labeled perfusion MRI for clinical applications: A consensus of the ISMRM perfusion study group and the European consortium for ASL in dementia [J]. Magn Reson Med, 2015, 73(1): 102-16.
[5] SCHEFFER I E, BERKOVIC S, CAPOVILLA G, et al. ILAE classification of the epilepsies: Position paper of the ILAE Commission for Classification and Terminology [J]. Epilepsia, 2017, 58(4): 512-21.
[6] WANG X, DING D, ZHAO Q, et al. Brain hemodynamic changes in amnestic mild cognitive impairment measured by pulsed arterial spin labeling [J]. Aging (Albany NY), 2020, 12(5): 4348-56.
[7] MELETTI S, MONTI G, MIRANDOLA L, et al. Neuroimaging of status epilepticus [J]. Epilepsia, 2018, 59 Suppl 2(113-9.
[8] SHIMOGAWA T, MORIOKA T, SAYAMA T, et al. The initial use of arterial spin labeling perfusion and diffusion-weighted magnetic resonance images in the diagnosis of nonconvulsive partial status epileptics [J]. Epilepsy Res, 2017, 129(162-73.
[9] LEIVA-SALINAS C, QUIGG M, ELIAS W J, et al. Earlier seizure onset and longer epilepsy duration correlate with the degree of temporal hypometabolism in patients with mesial temporal lobe sclerosis [J]. Epilepsy Res, 2017, 138(105-9.
[10] AKMAN C I, ICHISE M, OLSAVSKY A, et al. Epilepsy duration impacts on brain glucose metabolism in temporal lobe epilepsy: results of voxel-based mapping [J]. Epilepsy Behav, 2010, 17(3): 373-80.
Figures
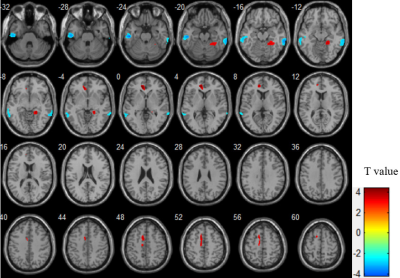
Figure 1 Brain regions that showed significant rCBF differences between EP group and HC group (P < 0.05, cluster-level, AlphaSim corrected). Hot and cool colors represent significantly increased and decreased rCBF in EP group, respectively. The T-value bar was shown on the right.
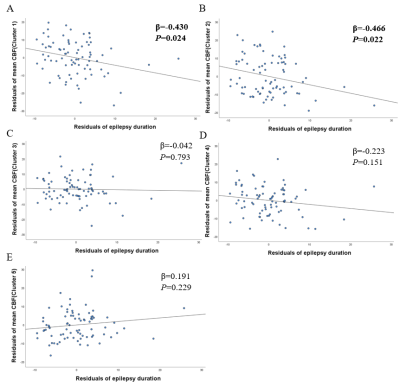
Figure 2 Partial regression plots demonstrating the influence of duration of epilepsy on mean CBF of Cluster 1-5 (Figure A-E).
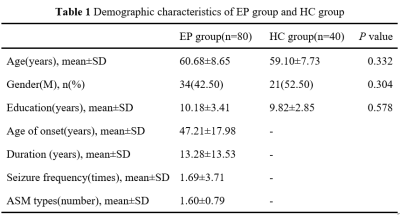
Abbreviation: ASM, anti-seizure medication
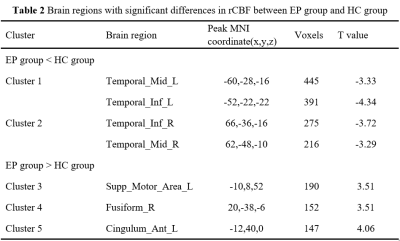
P < 0.05, cluster-level, AlphaSim corrected.
Abbreviations: Temporal_Mid_L: left middle temporal gyrus; Temporal_Inf_L: left inferior temporal gyrus; Temporal_Inf_R: right middle temporal gyrus; Temporal_Mid_R: right inferior temporal gyrus; Supp_Motor_Area_L: left supplementary motor area; Fusiform_R: right fusiform gyrus; Cingulum_Ant_L: left anterior cingulate and paracingulate gyri
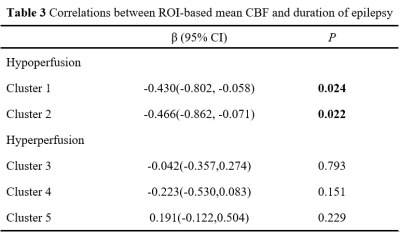
Adjusted for age of onset, gender, education, seizure frequency and number of anti-seizure medication types