5201
Quantification of Lesion Volume Differences in Structural Epilepsy in 7T and 3T1Department of Neurosurgery, Medical University of Vienna, Vienna, Austria, 2High-field MR Center, Department of Biomedical Imaging and Image-guided Therapy, Medical University of Vienna, Vienna, Austria, 3Division of Neuroradiology and Musculoskeletal Radiology, Department of Biomedical Imaging and Image-guided Therapy, Medical University of Vienna, Vienna, Austria, 4Department of Neurology, Hietzing Hospital, Vienna, Austria, 5Center for Rare and Complex Childhood Onset Epilepsies, Member of ERN EpiCARE, Department of Pediatrics and Adolescent Medicine, Medical University of Vienna, Vienna, Austria, 6Christian Doppler Laboratory for MR Imaging Biomarkers, Vienna, Austria, 7Department of Neurology, Medical University of Vienna, Vienna, Austria, 8Division of Nuclear Medicine, Department of Biomedical Imaging and Image-guided Therapy, Medical University of Vienna, Vienna, Austria
Synopsis
Keywords: Epilepsy, High-Field MRI
In this study, structural lesions in 3T and 7T of 12 patients suffering from intractable focal epilepsy were co-registered and manually segmented using ITK-SNAP. The rendered volumes were compared with reference to 3T lesional size in FLAIR, T1 and T2-weighted sequences. Additionally, a WMS sequence was compared to 3T FLAIR as well as 7T FLAIR. Our findings illustrate that on average, 7T showed larger lesion volume in all sequences except WMS.Introduction
Identification and precise delineation of structural lesions in pharmaco-resistant epilepsy are essential in surgical planning and increasing the probability of achieving postoperative seizure freedom1. Recently, numerous studies have shown superiority of 7T MRI over 3T MRI with regards to lesion detection and delineation2,3,4. The purpose of this study is to quantify volume differences and offer insight into qualitative parameters that may influence overall 7T performance over clinical routine MRI.Methods
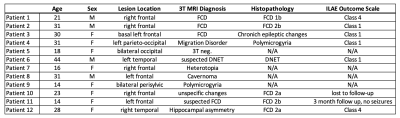
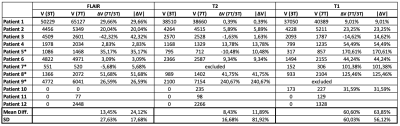
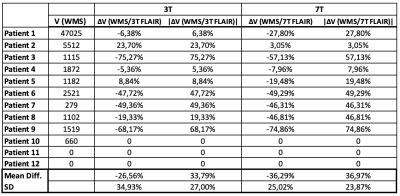
12 patients (8 females, 4 males, mean age 25±9 years) with intractable structural focal epilepsy that had undergone 3 and 7T MRI, as well as extensive presurgical evaluation were admitted (see Table 1). This included video monitoring (semiology of seizure onset, ictal and interictal EEG), [18F]FDG PET and 3T MRI. Inclusion criteria were: informed written consent, age ≥ 12 years and the presence of a structural lesion confirmed either by 3T MRI or by histopathology. Weight < 30 kg, claustrophobia, pregnancy, breastfeeding, and ferromagnetic implants led to exclusion from study participation. Of these patients, 8 had surgery later, thereby warranting histopathological confirmation of radiological diagnosis. The consensus protocol proposed by the 7T Epilepsy Task Force 20215 was used, with corresponding 3T images co-registered for comparison. This protocol was acquired with a Siemens Healthineers scanner with a 32-channel receive head coil (Nova Medical) and consisted of 3D T1w (Tacq=8:02min, resolution=0.75×0.75×0.75mm³); 3D T2w (Tacq=7:02min, resolution= 0.7×0.7×0.7mm³); coronal hippocampal T2w (Tacq=6:07min, resolution= 0.5×0.4×2.0mm³); 3D T2w fluid-suppressed (Tacq=12:18min, resolution= 0.9×0.9×0.9mm³) and 3D T2w fluid- and white matter-suppressed (Tacq=3:54min, resolution= 0.9×0.8×1.0mm³) MRI. The lesions had been previously identified by two neuroradiologists, blinded to clinical presentation in a first round, which laid the basis for delineation in segmentation. The patients’ corresponding 3T and 7T sequences were co-registered in ITK-SNAP6 and lesions were manually segmented in coronal, sagittal and transverse slices. Correct delineation was subsequently confirmed by a neuroradiologist. Due to the limited case number, descriptive statistics such as mean volume difference and standard deviation were calculated per sequence (FLAIR, T2w and T1w) and field strength, as well as for WMS compared to 3T and 7T FLAIR (due to lack of availability of 3T WMS data). As a reference for comparison, mean lesion difference was calculated relative to 3T lesion volume, illustrated in Table 2. The two patients with histopathologically confirmed structural epilepsy yet MRI-negative 3T images were included to assess lesion detectability on 7T.Results
7T MRI showed increased mean lesion volume over all sequences and in almost all patients, exceptions found only in those without histopathological verification (marked with asterisks), in which the significance of the lesion in terms of cause or consequence remains unclear and in Patient 3, where B1+ inhomogeneities significantly impeded on delineation of the basally located lesion. Breaking down volume difference per sequence, 7T FLAIR sequences showed a mean volume increase of 13% in comparison to 3T, whereas lesion volume was most similar over both field strengths in T2w images, averaging at 8% larger in 7T. The most substantial increase (as well as the largest standard deviation) was observed in T1w images, in which mean lesion volume was 61% larger on 7T. Contrary to the above findings, the WMS sequence showed smaller lesion size in comparison to 3T FLAIR (-27%) and 7T FLAIR (-36%). In the two 3T MRI-negative patients, the subtle lesions could be identified in all sequences other than WMS.Discussion and Conclusion
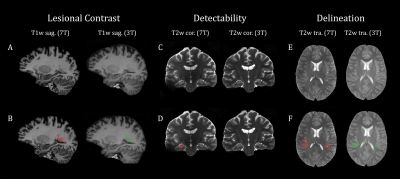
Our study shows that 7T consistently rendered larger lesional volumes compared to 3T in all sequences, especially T1, with the exception of the WMS sequence. However, the large standard deviation found throughout reveals that factors not taken into account in this study impact volume difference in 3T and 7T. An explanation for this may be the heterogeneity of pathologies and lesional location in our small patient population, stratifying volume differences according to these two factors in a larger cohort may lend insight into their influence on lesional size difference.The two patients with non-lesional 3T MRI were operated on in accordance with conclusive findings in extensive presurgical evaluation and not on the basis of 7T diagnosis and are therefore not representative for general lesion detectability in 3T-negative structural epilepsy. The focus of this study was to evaluate the relative volume difference of epileptogenic lesions in 7T versus 3T, however merely taking this parameter into account is insufficient in assessing overall 7T performance. Therefore, Figure 5 offers an overview of qualitative parameters such as improved lesional contrast, detectability and delineation that greatly influence the judgment of lesions. A current limitation of 7T sequences at our scanner are the basal B1+ inhomogeneities seen in all patients, impeding on interpretability of lesions in the temporal lobe as well as the small patient population.Acknowledgements
This study was supported by Neuroscience Cluster Seed Grants 2021 of the Medical University of Vienna Medical and the Medical-Scientific Fund of the Mayor of the Federal Capital Vienna (Project Number 21186).References
1. Ryvlin P, Cross JH, Rheims S. Epilepsy surgery in children and adults. Lancet Neurol. 2014;13(11):1114-1126. doi:10.1016/S1474-4422(14)70156-5
2. van Lanen, R. H. G. J., Wiggins, C. J., Colon, A. J., Backes, W. H., Jansen, J. F. A., Uher, D., ... & Schijns, O. E. M. G. (2022). Value of ultra-high field MRI in patients with suspected focal epilepsy and negative 3 T MRI (EpiUltraStudy): protocol for a prospective, longitudinal therapeutic study. Neuroradiology, 64(4), 753-764. doi:10.1007/s00234-021-02884-8
3. Veersema, T. J., Ferrier, C. H., van Eijsden, P., Gosselaar, P. H., Aronica, E., Visser, F., ... & Braun, K. P. (2017). Seven tesla MRI improves detection of focal cortical dysplasia in patients with refractory focal epilepsy. Epilepsia Open, 2(2), 162-171. doi:10.1002/epi4.12041
4. Park JE, Cheong EN, Jung DE, Shim WH, Lee JS. Utility of 7 Tesla Magnetic Resonance Imaging in Patients With Epilepsy: A Systematic Review and Meta-Analysis. Front Neurol. 2021;12:621936. doi:10.3389/fneur.2021.621936
5. Opheim G, van der Kolk A, Bloch KM, et al. 7T Epilepsy Task Force Consensus Recommendations on the Use of 7T MRI in Clinical Practice. Neurology. 2021;96(7):327-341. doi:10.1212/WNL.0000000000011413
6. Paul A. Yushkevich, Joseph Piven, Heather Cody Hazlett, Rachel Gimpel Smith, Sean Ho, James C. Gee, and Guido Gerig. User-guided 3D active contour segmentation of anatomical structures: Significantly improved efficiency and reliability. Neuroimage 2006 Jul 1;31(3):1116-28.
Figures