4989
Applicability of Magnetic Resonance Fingerprinting for Proton Resonance Frequency Shift based Temperature Monitoring of Microwave Ablation
Moritz Gutt1, Josef Joaquin Löning Caballero2, Dominik Horstmann2, Frank Wacker2, Bennet Hensen2, and Marcel Gutberlet2
1Computational Health Informatics, Leibniz University Hannover, Hannover, Germany, 2Diagnostic and Interventional Radiology, Hannover Medical School, Hannover, Germany
1Computational Health Informatics, Leibniz University Hannover, Hannover, Germany, 2Diagnostic and Interventional Radiology, Hannover Medical School, Hannover, Germany
Synopsis
Keywords: Thermometry, MR Fingerprinting
MRI offers the unique ability of measuring the temperature inside of the patient during minimally invasive tumor ablation. In this proof-of-concept approach MR Fingerprinting was used in order to get an accurate thermometry with potential for real-time application. The method was validated by performing a microwave ablation in a bioprotein phantom. The temperature accuracy was 1.54 °C ± 0.85 °C and the dice score between the calculated and the ground truth denaturation zone was 90.02 %. The mean standard deviation of the non-heated area was 0.19 °C.Introduction
Magnetic Resonance Fingerprinting (MRF) is a framework which can be utilized to acquire multiple quantitative parameter maps at once whilst being relatively fast compared to other quantitative methods1. MRF assumes that, given the right pulse sequence, tissue generates a unique signal evolution based on its underlying parameters. The measured signal can therefore be matched with a pregenerated dictionary in order to acquire the quantitative parameter maps.In clinical practice, MR guided temperature monitoring during minimally invasive tumor ablation is an important topic. However, a high accuracy in estimating the temperature as well as the resulting necrosis zone is needed to provide a real impact on the clinical routine. Due to the high error tolerance1 of the matching process and the ability to quantize multiple parameters at once, MRF might be a promising framework to use here.
Typically, MRF reconstruction times are rather high due to the size of the dictionary. In the case of temperature monitoring during tumor ablation however, the dictionary size can be kept small, since only a rather small range of temperature changes is possible between two time steps. This could allow for real-time reconstruction with MRF.
In this proof-of-concept approach, the applicability of MRF in proton resonance frequency shift (PRFS) based temperature monitoring of microwave ablation (MWA) is shown by measuring the B0 off-resonance.
Methods
For data acquisition a 2D multi-echo radial FLASH sequence was used. In order to achieve additional sensitivity to the B0 off-resonance, the echo times were varied with every TR. Thus, the total range of TEs was between 2.57 ms and 29.11 ms with a step size of 0.336 ms, leading to 80 different echo times. The field of view was 320 x 320 mm2 with a resolution of 256 x 256 and a slice thickness of 5 mm. The dictionary consisted of off-resonance values corresponding to temperature changes between -1 °C and 40 °C with a step size of 0.1 °C. The dictionary entries were calculated by utilizing the linear dependency of the temperature and the proton resonance frequency of water between temperatures of -15 °C and 100 °C2. A small temperature decrease was allowed in order to measure and correct for the phase drift. For every echo time, 10 spokes were acquired such that the k-space was undersampled by a factor of 40. The temporal resolution was 2.9 s.The toolbox BART3 was used for reconstructing the data from each TE with parallel imaging and compressed sensing (PICS). After reconstruction, the dictionary matching process was performed by taking the highest inner product between the reconstructed signals and the dictionary entries. Additionally, a denaturation map was calculated by the CEM434 model. In order to verify this proof-of-concept, a microwave ablation (modified ECO-100E, Eco Microwave System Co., Ltd., Nanjing, China, 2.45 GHz, 150 W) on a static bioprotein phantom5 was performed on a 1.5 T scanner (Siemens Avanto) and monitored by the fingerprinting sequence. A fiber optical temperature sensor was used for gaining reference temperatures. The sensor had a distance of approx. 1 cm to the ablation needle. After the ablation, manual segmentation of the denaturation zone in a post-ablative T2-weighted Turbo-Spin-Echo sequence (TE=156 ms, TR=10960 ms) was done and used as a ground truth for comparison with the calculated denaturation map.
Results
The fingerprinting method achieved a temperature accuracy of 1.54 °C ± 0.85 °C compared to the temperature sensor. An example of a temperature map from the MRF reconstruction is shown in Figure 1. Figure 4 shows the calculated temperature development compared to the actual temperature. The mean standard deviation of the non-heated area was 0.19 °C. The comparison of the denaturation zone with the ground truth (see Figure 3) yielded a dice score of 90.02%.Discussion
This proof-of-principle approach has shown that MRF is a promising tool for temperature monitoring and further research should be done to discover its full potential. In future studies an MRF sequence which is additionally sensitive to T1 relaxation could be utilized to simultaneously quantize the B0 off-resonance and T1 and therefore be able to monitor the temperature of adipose tissue as well. Furthermore, one could make use of the body heat equation to further restrict the dictionary entries and achieve a more precise result. Additionally, a more efficient k-space sampling like a spiral readout could be used to improve the temporal resolution and the reconstruction time could be improved by replacing the dictionary matching with a neural network.Acknowledgements
No acknowledgement found.References
1. POORMAN, ME et al; JMRI 2020;51:675–692
2. RIEKE, V et al; JMRI 2008 27(2) 376–390
3. UECKER, M et al; Proc. Intl. Soc. Mag. Reson. Med. 23 (2015), S. 2486
4. PEARCE, JA et al; International Journal of Hyperthermia 29 (2013), Nr. 4, S. 262–280
5. BU-LIN, Z et al; International Journal of Hyperthermia 2008 24(7) 568–576
Figures

Figure 1: A temperature map generated with the MRF reconstruction
Figure 2: Magnitude image of the phantom with the ablation needle and the optical temperature sensor
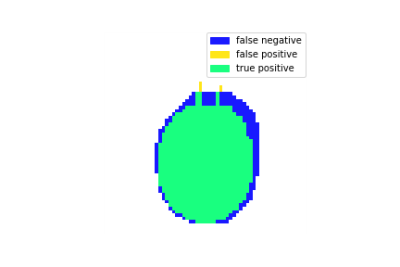
Figure 3: Denaturation zone calculated with the MRF temperature maps
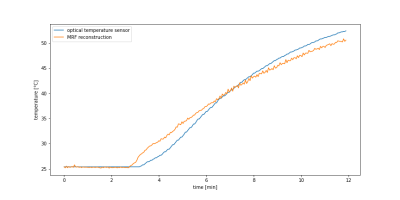
Figure 4: Calculated temperature compared to the temperature measured by the optical temperature sensor
DOI: https://doi.org/10.58530/2023/4989