4986
A clinical application of deep learning reconstructed myocardial late gadolinium enhancement on short-breath-hold patients1Department of Radiology, Renmin Hospital of Wuhan University, Wuhan, China, 2GE Healthcare, MR Research China, Beijing, China, 3General Electric Medical (China) Co, Beijing, China
Synopsis
Keywords: Myocardium, Image Reconstruction
SNR and CNR are essential for radiologists to precisely assess the signal enhancement in myocardia tissues. High-resolution late gadolinium enhancement cardiac magnetic resonance (LGE-CMR) is important but often possess low SNR and takes long scan time. Compared with original PSMDE (PSMDEO), AIRTM Recon DL-based PSMDE (PSMDEDL) effectively and significantly improved SNR, CNR and image quality without extra scan time. High-resolution PSMDEDL images also accelerated diagnossis speed of identifying defected tissues from noisy but normal myocardial tissues and elevated the diagnosis confidence despite no statistically different diagnostic performance between PSMDEDL and PSMDEO images.Purpose
Signal enhancement in phase sensitive myocardial delayed enhancement (PSMDE) sequences is a critical bioimage feature in the assessment and treatment of patients with troponin I (TnI)-positive acute chest pain in cardiovascular magnetic resonance (CMR). Accurate identification of signal enhancement requires sufficient signal to noise ratio (SNR) and contrast to noise ratio (CNR) [1-3]. Deep learning reconstruction (DLR) is an important application for medical image [4,5], allowing faster image acquisition (fewer number of excitations) especially for patients without capability of normal breath-hold (approximately 12 seconds), improving image quality and diagnostic performance on diseases particularly for radiologists with less experience in CMR, and eliminating intra- and inter-observer variation in interpretation. The aim of this study was to explore the value of DLR techniques in high-resolution free-breathing PSMDE sequence.Methods
This study was approved by our hospital (Approval No. 2022K-K083). A total of 48 chest pain patients with TnI-positive acute chest pain examined at our hospital from April to July 2022 were prospectively collected, including conventional short-axis cardiac scans of both PSMDE with conventional image reconstruction (PSMDEo) and PSMDEDL automatically post-processed with commercial AIRTM Recon DL (Signa Architect, GE Healthcare), for this study. Parameters of PSMDEo and PSMDEDL sequence were the same except for DL option shown in Table 1.All patients received adequate a respiratory training before scanning to avoid respiratory motion artefacts. Fifteen minutes ahead of scanning the PSMDEO and PSMDEDL sequences, gabexidine glucosamine injection (Modic, Shanghai Boris Pharmaceutical Co., Ltd.) was administered at 0.1 mmol/kg body weight at a flow rate of 3.5 ms/s and an equivalent amount of saline at the same flow rate.
The Likert scale and objective quantitative indices (SNR = mean of signal intensity (SI)/ standard deviation of SI and CNR = |SI-SI|/SD) were applied for subjective and objective evaluation of the image quality of PSMDEO and PSMDEDL sequences, respectively, Fig 1. The diagnostic efficacy included qualitative assessment of the presence or absence of foci reinforcement and reinforcement scoring of cases with reinforced foci. The subjective and objective evaluation were performed by two radiologists with more than 5 years of experience in the diagnosis of cardiovascular diseases. One of the radiologists reassessed the image quality of PSMDEO sequences and PSMDEDL sequences after 1 month for subjective and objective evaluation, diagnostic efficacy scores (including qualitative evaluation with or without enhancement and enhancement scores). SPSS (version 25.0, Chicago, IL) was used to analyze both intra- and inter-observer agreement of two image data set.
Results
In terms of subjective assessment, significantly higher scores of subjective image quality (4.31±0.83 vs. 3.98±0.70, P < 0.05) as well as better intra-group and inter-group consistency were found in the PSMDEDL group than the PSMDEO group. In terms of objective evaluation, PSMDEDL group had significantly higher SNR (60.10±34.36 vs. 31.04±8.35) and CNR (110.32±65.78 vs. 51.06±26.82) than the PSMDEO group (all P < 0.05), Fig 2, and the intra-group and inter-group consistencies were good (ICC > 0.700, P < 0.001). There were 39 patients (81.25%) with PSMDEDL sequence enhancement lesions and 41 patients (85.42%) with PSMDEO sequence enhancement lesions, with no statistically significant difference in qualitative scores (t = -1.43, P > 0.05). There was no statistically significant difference of enhancement scores between PSMDEDL and PSMDEO ((11.06 ± 9.74 vs.10.54 ± 9.81, P > 0.05) and the intra- and interobserver agreement was good (weighted kappa > 0.800, P < 0.001) (Table 2).Discussion and conclusions
Both PSMDEO and PSMDEDL images were obtained at one scan without prolonging PSMDE scan timepoints and can assist clinical diagnosis with high reliability especially in concerning about missing defected tissues. In clinical work, approximately one-thirds of patients do not possess a stable heart rate and cannot control respiratory rhythm, leading to poor image quality of PSMDE. When the diastolic phase is short, PSMDE images are possibly blurred, not to mentioned high myocardial SNR and CNR. A deep convolutional neural network (CNN) model was embedded into the raw data reconstruction pipeline to improved SNR and CNR via effective separation of signals and noises and diagnostic efficacy was not compromised [6-7]. The CNN reconstruction is a very effective tool in noise suppression with good performance. PSMDE sequence itself is sensitive to cardiovascular motion [8-9]; that is, vascular motion and blood stasis in the lumen lead to myocardial signal loss and low SNR. A common strategy of increasing layer thickness elevates SNR and brings about unwanted signals caused by slow blood flow and lager excitation volume effects, leading to reduce sensitivity to lesions and CNR. Therefore, applications of DLR in CMR is effective and essential for clinics [10]. The patients enrolled in this study had heavy symptoms, but the average subjective image quality score of the PSMDEDL sequence was high (4.31±0.83) with good SNR and CNR, indicating that PSMDEDL is highly potential usage in clinicals.Acknowledgements
No acknowledgement found.References
[1] Curfman G. Acute Chest Pain in the Emergency Department. JAMA Intern Med ,2018,178(2):220. DOI: 10.1001/jamainternmed.2017.7519.
[2] Liu B, Dardeer AM, Moody WE, et al. Reference ranges for three-dimensional feature tracking cardiac magnetic resonance: comparison with twodimensional methodology and relevance of age and gender. Int J Cardiovasc Imaging, 2018, 34(1):761-775. DOI: 10.1007/s10554-017-1277-x.
[3] Dastidar AG, Baritussio A, De Garate E, et al. Prognostic role of CMR and conventional risk factors in myocardial infarction with nonobstructed coronary arteries. JACC Cardiovasc Imaging, 2019,12(10):1973–1982. DOI: 10.1016/j.jcmg.2018.12.023.
[4] Pesapane F, Codari M, Sardanelli F, et al. Artificial intelligence in medical imaging: threat or opportunity? Radiologists again at the forefront of innovation in medicine. Eur Radiol Exp, 2018,2(1):1-10. DOI: 10.1186/s41747-018-0061-6.
[5] Silvia Pradella, Lorenzo Nicola Mazzoni, Mayla Letteriello, et al. FLORA software: semi-automatic LGE-CMR analysis tool for cardiac lesions identification and characterization. Radiol Med, 2022,127(6):589-601. DOI: 10.1007/s11547-022-01491-8.
[6] Nikki van der Velde,H. Carlijne Hassing,Brendan J. Bakker, et al. Improvement of late gadolinium enhancement image quality using a deep learning–based reconstruction algorithm and its influence on myocardial scar quantification. Eur Radiol,2021,31(6):3846–3855. DOI:10.1007/s00330-020-07461-w.
[7] Muscogiuri G, Martini C, Gatti M, et al. Feasibility of late gadolinium enhancement (LGE) in ischemic cardiomyopathy using 2D-multisegment LGE combined with artificial intelligence reconstruction deep learning noise reduction algorithm[J]. Int J Cardiol,2021,369(12):164-170. DOI:10.1016/j.ijcard.2021.09.012.
[8] Zhang Y, Zhu Y, Zhang K, et al. Invasive ductal breast cancer: preoperative predict Ki-67 index based on radiomics of ADC maps[J]. Radiol Med, 2020, 125(2): 109-116. DOI: 10.1007/s11547-019-01100-1.
[9] Brandão LA, Young Poussaint T. Posterior Fossa Tumors[J]. Neuroimaging Clin N Am, 2017, 27(1): 1-37. DOI: 10.1016/j.nic.2016.08.001.
[10] Solenn Toupin, Théo Pezel, Aurélien Bustin, et al. Whole-Heart High-Resolution Late Gadolinium Enhancement: Techniques and Clinical Applications. J Magn Reson Imaging,2022,55(4):967-987. DOI: 10.1002/jmri.27732.
Figures
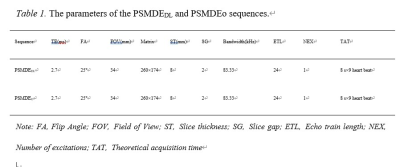
Table 1. The parameters of the PSMDEDL and PSMDEo sequences.
Note: FA, Flip Angle; FOV, Field of View; ST, Slice thickness; SG, Slice gap; ETL, Echo train length; NEX, Number of excitations; TAT, Theoretical acquisition time.
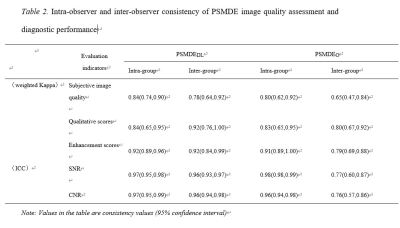
Table 2. Intra-observer and inter-observer consistency of PSMDE image quality assessment and diagnostic performance
Note: Values in the table are consistency values (95% confidence interval).
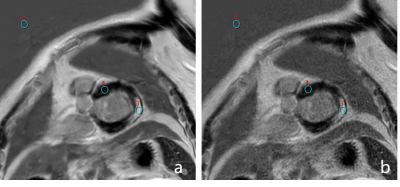
Fig. 1. a. PSMDEDL sequence, b. PSMDEO sequence. ROI1. Normal myocardial ROI, ROI2. Background ROI, ROI3. Compared with panel b, panel a is clearer, with less noise, more uniform signal from normal myocardium, and greater contrast between enhanced foci and normal myocardium.
Note: ROI, region of interest.
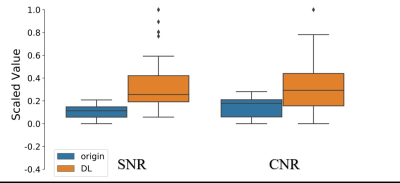
Fig. 2. SNR and CNR of Original PSMDE (PSMDEO) and AIRTM Recon DL-based PSMDE (PSMDEDL). SNR and CNR significantly improved without extra scan time. The vertical coordinate indicates the normalised value.
Note: DL, deep learning. SNR, signal to noise ratio. CNR, contrast to noise ratio.