4912
Deep Learning Based Real-time Quality Assessment of Pilot Tone Respiratory Signals
Huixin Tan1 and Yantu Huang1
1Siemens Shenzhen Magnetic Resonance Ltd., China, Shenzhen, China
1Siemens Shenzhen Magnetic Resonance Ltd., China, Shenzhen, China
Synopsis
Keywords: Machine Learning/Artificial Intelligence, Machine Learning/Artificial Intelligence
Pilot Tone (PT) respiratory signals are susceptible to interference like patient bulk motion or radio frequency interference. The signal curve is prone to bad when remains strong interference after suppression processing in the learning phase, resulting in low triggering accuracy and efficiency. With real-time quality assessment in the learning phase, a good-quality signal can be selected to learn better processing parameters. To ensure robustness and inference time, a tiny CNN is utilized to classify the signal into good and bad quality. Experimental results demonstrate that the proposed method has a strong ability to assess the quality of PT respiratory signals.Summary of Findings
Pilot Tone respiratory signals can be improved by the deep learning quality assessment model, thereby improving the performance of the Pilot Tone respiratory triggering.Introduction
Pilot Tone (PT) navigation1 is a novel and promising technique in abdominal and cardiac MR scans. A PT respiratory signal with bad quality can lead to low accuracy and efficiency of the triggering, resulting in the deterioration of MR image quality and long scan time. At the beginning of a measurement, processing parameters are obtained, including the channel combination coefficients used to transform the multi-channel PT raw data into a PT respiratory signal, the RF interference suppression, the sign of the respiratory signal, the scaling ratio, etc., named as learning phase. When the learning finishes, triggering begins, named as triggering phase. The PT respiratory signal in the triggering phase is synthesized by the learned processing parameters. If the signal quality in the learning phase is bad, the learned processing parameters may not be accurate, resulting in a bad curve and wrong or missing triggers in the triggering phase. Thus, the quality assessment of the PT respiratory signal in the learning phase is significant.Currently, most of the quality assessment methods of respiratory signals are aimed at improving the performance of respiration monitoring. Traditional features like respiratory quality indices2-4 are the most common way to assess the quality of respiratory signals but suffer from less robustness. Machine learning based methods5-7 take the traditional features as input. Different from setting rules artificially, machine learning based methods can learn the classification bounder according to the training data. Both methods rely on feature extraction and selection, which is not robust enough when comes to complicated scenarios. Besides, the features are not designed for respiratory triggering technology. In this work, we propose to apply a robust CNN model to assess the quality of PT respiratory signals for promoting the performance of the PT respiratory triggering.
Methods
The dataset is collected from 228 volunteers on the 0.55/1.5 T MR scanner (MAGNETOM Free.Star/Free.Max/Amira, Siemens Healthineers). 6306 signals of 30 volunteers in the triggering phase are labeled as pretraining dataset. 1760 signals of all volunteers in the learning phase are labeled as training dataset.The whole PT respiratory signal is filtered by the Kalman filter and then is downsampled from 2000 Hz to 125 Hz to reduce the computational complexity of the model. Since the time of the learning phase is 12s, the whole PT respiratory signal is segmented into many segments of 12s. At last, min-max normalization is utilized to normalize the segmented signal.
Due to the imbalance of our dataset, that the number of good-quality signals are much more than bad-quality signals, 4 signal augmentation methods shown in Figure 1 are adopted to improve the training stability and relieve overfitting.
A tiny CNN of Resnet8 type shown in Figure 2 is designed to assess the quality of PT respiratory signals in real time. Resnet is proposed to ease the training of the deeper and wider network. Different from this purpose, we reduce the number of network layers and output channels per layer without following the suggested architecture form, making it shallower and narrower. Original Resnet has large model parameters, but our tiny Resnet only has 0.08M. On one hand, tiny architecture can ensure the real-time requirement of quality assessment of PT respiratory signals. On the other hand, current dataset is too small to train a big CNN model well. The model is firstly pretrained by the signals in the triggering phase and then finetuned by the signals in the learning phase.
Results and Discussion
Due to the small scale of the dataset, the experiment was conducted in 10-fold cross-validation. Results demonstrated in Table 1 and 2 show the great performance of the proposed method, not only for the quality assessment in the learning phase (98.01% accuracy) but also for the quality assessment in the triggering phase (99.45% accuracy), meaning that the model trained on the data of the triggering phase can also be used to detect bad-quality PT respiratory signals so that the clinical operator can be reminded of these.Besides, the inference time on the i7-11850H CPU of the model is ~3ms, which can meet the requirement of real-time quality assessment.
To further prove the effectiveness of the quality assessment model, extra 22 volunteers were tested. Results are illustrated in Table 3 and 4.
With the quality assessment in the learning phase, the respiratory curve and the triggering accuracy and efficiency can be improved. As Figure 3 shows, with quality assessment, the bad-quality segment can be discarded, and then the good-quality segment can be chosen in the learning phase, resulting in a better curve and accurate triggers. Overall, 13 PT respiratory signals in the whole triggering phase are bad in this test, of which 9 signals (about 70%) have been corrected with our method. The left 30% bad signals are caused by patient motion in the triggering phase, and this situation cannot be improved so far.
Conclusion
Proposed method can precisely assess the quality of PT respiratory signals in real time, thereby improving the respiratory curve and the triggering accuracy and efficiency of the PT triggering.Acknowledgements
No acknowledgement found.References
- Speier P, Fenchel M. and Rehner R. PT-Nav: a novel respiratory navigation method for continuous acquisitions based on modulation of a pilot tone in the MR-receiver. Magn Reson Mater Phys Biol Med. 2015, 28: S97-S98. doi: 10.1007/s10334-015-0487-2.
- Birrenkott D. Respiratory quality index design and validation for ECG and PPG derived respiratory data. Report for transfer of status, Dept. Eng. Sci., Univ. Oxford, Oxford, UK. 2015.
- Birrenkott DA, Pimentel MA, Watkinson PJ, & Clifton DA. Robust estimation of respiratory rate via ECG-and PPG-derived respiratory quality indices. Annu Int Conf IEEE Eng Med Biol Soc (EMBC). 2016, 676-679. doi: 10.1109/EMBC.2016.7590792.
- Birrenkott DA, Pimentel MA, Watkinson PJ, & Clifton DA. A robust fusion model for estimating respiratory rate from photoplethysmography and electrocardiography. IEEE Trans Biomed Eng. 2017, 65(9), 2033-2041. doi: 10.1109/TBME.2017.2778265.
- Charlton PH, Bonnici T, Tarassenko L, Clifton DA, Beale R, Watkinson PJ, & Alastruey J. An impedance pneumography signal quality index: Design, assessment and application to respiratory rate monitoring. Biomed Signal Process Control. 2021, 65: 102339. doi.org/10.1016/j.bspc.2020.102339.
- Rozo A, Moeyersons J, Morales J, van der Westen RG, Lijnen L, Smeets C, ... & Varon C. Data Augmentation and Transfer Learning for Data Quality Assessment in Respiratory Monitoring. Front Bioeng Biotechnol. 2022, 10: 806761. doi: 10.3389/fbioe.2022.806761.
- Xu H, Yan W, Lan K, Ma C, Wu D, Wu A, ... & Zhang Z. Assessing electrocardiogram and respiratory signal quality of a wearable device (sensecho): semisupervised machine learning-based validation study. JMIR mHealth and uHealth. 2021, 9(8): e25415. doi: 10.2196/25415.
- He K, Zhang X, Ren S. and Sun J. Deep residual learning for image recognition. Proc IEEE Comput Soc Conf Comput Vis Pattern Recognit. 2016, 770-778. doi: 10.1109/CVPR.2016.90.
Figures

Figure 1: Four signal augmentation methods: (a) Original signal. (b)
Scaling. (c) Cropping and resizing. (d) Flipping left and right. (e) Flipping
up and down.
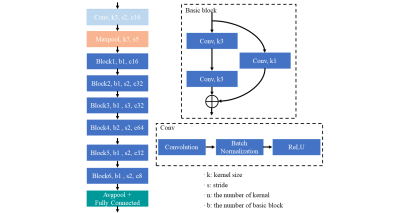
Figure 2: Network architecture of the tiny CNN of Resnet type.
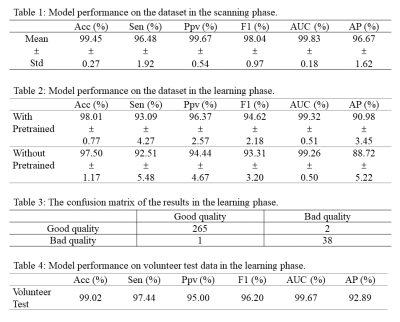
Table 1-4.
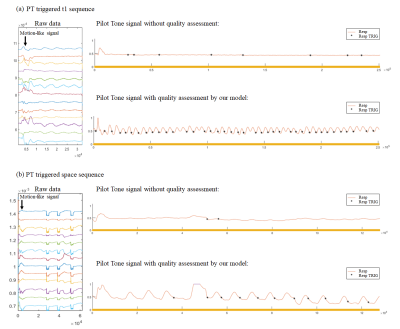
Figure 3: The improvement of the PT respiratory signal with our method.
DOI: https://doi.org/10.58530/2023/4912