4869
Effect of Left Ventricular Myocardial Strain on Right Ventricle in Hypertrophic Cardiomyopathy1Taiyuan Central Hospital of Shanxi Medical University, Taiyuan, China, 2Department of MR Scientific Marketing, Siemens Healthineers Ltd., Beijing, China
Synopsis
Keywords: Myocardium, Cardiomyopathy, Hypertrophic cardiomyopathy, Biventricular function
This study evaluated the right ventricular (RV) myocardial strain of Hypertrophic Cardiomyopathy (HCM) patients with preserved ejection fraction (EF) and without myocardial hypertrophy in RV based on Cardiovascular magnetic resonance feature tracking technique (CMR-FT), and further explored the effect of left ventricular (LV) myocardial mechanics on the RV. The results showed that the global longitudinal strain (GLS) of the RV has been impaired, although the structure and EF of the RV were normal, so myocardial strain can be more sensitive and earlier to identify cardiac impairment. The systole function of the LV has a great influence on the RV function.
Introduction
Radiologic diagnosis of Hypertrophic Cardiomyopathy (HCM) is based on left ventricular (LV) wall hypertrophy. Currently, HCM research mainly focuses on the function of the LV [1]. Myocardial systole function of HCM is usually assessed by ejection fraction (EF). The EF of HCM is often normal or increased, while the decrease of EF does not occur until the late stage of the disease. The clinical treatment of HCM apply negative inotropic drugs to relieve the diastolic function of the LV, while ignoring the systolic function.Recent studies have found that right ventricular (RV) function is independently associated with prognosis in HCM[2,3], but few studies have been focused on the RV function in the past, especially for HCM patients without RV structure involvement. The LV and RV are integrated, whether the systolic and / or diastolic function of LV affects RV has not been reported[4]. Therefore, this study was to evaluate the myocardial strain of the RV in HCM without RV involvement, and further explore the effect of LV systolic and / or diastolic function on RV to further guide clinical treatment.
Methods
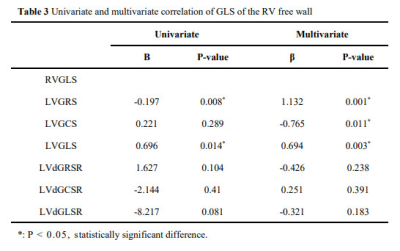
There were 30 patients of HCM and 24 healthy volunteers were included, which were divided into HCM group and control group. HCM group had no RV hypertrophy (end-diastolic wall thickness of RV ≤ 5 mm), preserved EF (LVEF ≥ 50%, RVEF > 45%) and no other cardiac, systemic or metabolic disease. All subjects were examined with a 3T MR scanner (MAGNETOM Skyra, Siemens Healthcare, Erlangen, Germany) with an 18-channel phase array coil. A balanced steady-state free precession sequence (bSSFP) and prospective ECG trigger were used to acquire cardiac cine images within a breath hold at the end of expiration. Short-axis, two-chamber, three-chamber and four-chamber cardiac cine views were acquired (Figure 1). CVI software (version 5.12.2, Circle Vascular Imaging) was used to measure conventional cardiac function and maximal left ventricular end-diastolic wall thickness (LVEDWT) , and analyze the myocardial strain of the LV and RV. Myocardial strain parameters include global radial strain (GRS), global circumferential strain (GCS), global longitudinal strain (GLS), global systolic longitudinal strain rate (sGLSR), radial strain rate (sGRSR), circumferential strain rate strain rate (sGCSR), global diastolic longitudinal strain rate (dGLSR), radial strain rate (dGRSR), and circumferential strain rate (dGCSR) of left ventricle and the GLS, sGLSR and dGLSR of RV free wall of all subjects. Student's t test or the Mann‒Whitney U test were used to compare the myocardial strain between the two groups. The correlation between right and left ventricular myocardial strain in patients of HCM was evaluated by Spearman correlation analysis. The influence factors to RV-GLS were analyzed by multiple linear regression. All statistical analyses were performed by SPSS (v26, International Business Machines, Armonk, New York, USA).Results
Age, sex, body mass index (BMI) and heart rate (HR) were not significantly different between the two groups. Compared with the control group, LVEF, LVCI, LVMI, LVSVI and RVEF in the HCM group were significantly increased, and LVESVI and RVESVI were significantly decreased (Table 1). Compared with the control group, GRS, GLS, sGLSR, dGRSR, dGLSR of LV and GLS of RV were significantly decreased in the HCM group (Table 2). In HCM group, spearman correlation analysis showed that absolute value of RVGLS was positively correlated with LVGRS, absolute value of LVGLS and LVsGRSR (Figure 2). In multiple linear regression analysis, LVGRS, LV GCS and LVGLS jointly affected the RVGLS (adjusted R2 = 0.477, P < 0.05) (Table 3).Discussion
The pathological mechanisms of HCM are cardiomyocyte hypertrophy, disorder and interstitial fibrosis, which also occur in the RV [5,6], so RV strain was impaired without RV hypertrophy Effect of LV myocardial mechanics on RV may be caused by the following reasons: (1) anatomical structure and (2) hemodynamic effects. The ventricular septum, a shared part of the LV and RV, is mostly involved in HCM, and the myocardium at the continuation of the left and right ventricular myocardium is secondary to the contraction of the LV [7,8]. The LV systolic dysfunction leads to the increase of LV filling pressure, which further leads to the increase of left atrial pressure. The pressure passively propagates backward, leading to pulmonary vein and pulmonary artery hypertension, which affects RV function[9,10]. For the treatment of HCM, the traditional medical treatment is to use negative inotropic drugs, such as β- Blockers can slow down HR and improve diastolic dysfunction by prolonging LV filling time[11]. However, the results of this study show that LV systolic function has a great impact on RV, and RV function is related to the prognosis of HCM. Therefore, we suggest that the changes of HCM systolic function should be paid attention in clinical treatment to improve the prognosis of HCM.Conclusion
HCM with preserved EF and no myocardial hypertrophy in RV showed strain changes, myocardial strain can be more sensitive and earlier to identify cardiac impairment. The LV systolic function has a great influence on the RV function, and RV function is related to the prognosis of HCM. Therefore, we suggest that the changes of HCM systolic function in clinical treatment should be paid attention.Acknowledgements
No acknowledgement found.References
1. Maron BJ, Desai MY, Nishimura RA et al. (2022) Diagnosis and Evaluation of Hypertrophic Cardiomyopathy: JACC State-of-the-Art Review. J Am Coll Cardiol 79:372-389.
2. Seo J, Hong YJ, Kim YJ et al. (2020) Prevalence, functional characteristics, and clinical significance of right ventricular involvement in patients with hypertrophic cardiomyopathy. Sci Rep 10:21908.
3. Hiemstra YL, Debonnaire P, Bootsma M et al. (2019) Prevalence and Prognostic Implications of Right Ventricular Dysfunction in Patients With Hypertrophic Cardiomyopathy. Am J Cardiol 124:604-612.
4. Ding W, Bhushan S, Ma C, Yan Y, Xiao Z (2021) Right Ventricle Involvement in Hypertrophic Cardiomyopathy and Role of Cardiac Magnetic Resonance in Hypertrophic Cardiomyopathy: Review Article. Heart Surg Forum 24:E746-e750.
5. Marian AJ (2021) Molecular Genetic Basis of Hypertrophic Cardiomyopathy. Circ Res 128:1533-1553.
6. Berger SG, Sjaastad I, Stokke MK (2021) Right ventricular involvement in hypertrophic cardiomyopathy: evidence and implications from current literature. Scand Cardiovasc J 55:195-204.
7. Buckberg G, Hoffman JI (2014) Right ventricular architecture responsible for mechanical performance: unifying role of ventricular septum. J Thorac Cardiovasc Surg 148:3166-3171.e3161-3164.
8. Ho SY, Nihoyannopoulos P (2006) Anatomy, echocardiography, and normal right ventricular dimensions. Heart 92 Suppl 1:i2-13.
9. Kovacheva E, Gerach T, Schuler S, Ochs M, Dössel O, Loewe A (2021) Causes of altered ventricular mechanics in hypertrophic cardiomyopathy: an in-silico study. Biomed Eng Online 20:69.
10. Ma G, Xu M, Gao W et al. (2014) Left ventricular filling pressure assessed by exercise TDI was correlated with early HFNEF in patients with non-obstructive hypertrophic cardiomyopathy. BMC Cardiovasc Disord 14:194.
11. Maron BJ, Desai MY, Nishimura RA et al. (2022) Management of Hypertrophic Cardiomyopathy: JACC State-of-the-Art Review. J Am Coll Cardiol 79:390-414.
Figures
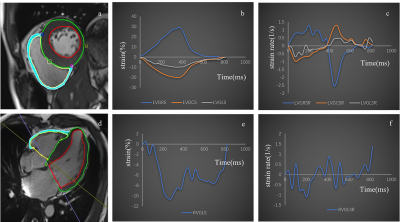
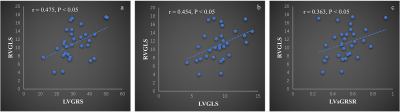
Figure 2. Correlation of global strain between the LV and RV. The absolute value of RVGLS was positively correlated with LVGRS (r = 0.475, P < 0.05) (a), the absolute value of LVGLS (r = 0.454, P < 0.05) (b), and LVsGRSR (r = 0.363, P < 0.05) (c).
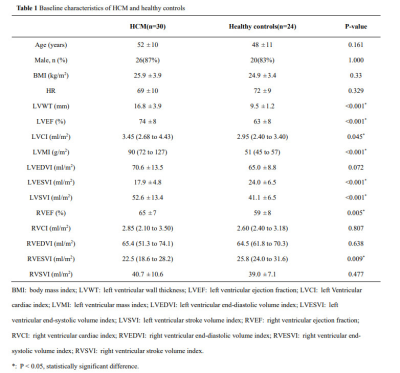
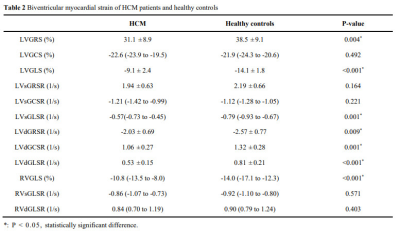
Table 2 Biventricular myocardial strain of HCM patients and healthy controls