4865
Analysis of Biventricular and Biatrial Strain by Cardiovascular Magnetic Resonance in Dilated Cardiomyopathy1The Second Affiliated Hospital of Harbin Medical University, Harbin, China, 2Philips Healthcare, Beijing, China
Synopsis
Keywords: Cardiomyopathy, Myocardium, strain, feature tracking, fast long-axis
Dilated cardiomyopathy (DCM) remains to attract worldwide attention for its poor prognosis and high mortality. The interaction of biatrial and biventricular deformation capacity in DCM patients is unclear. In this study, feature tracking and fast long-axis method were used to evaluate myocardial strain. We found that biventricular and biatrial strain were significantly impaired in DCM group than control group. LV GLS was obviously impaired in event group than no event group, and it showed significantly prognostic value in predicting cardiovascular events. Comprehensive CMR analysis should be performed to improve the diagnosis ability for DCM patients.Introduction
Dilated cardiomyopathy (DCM) remains to be a demanding issue because the facilitation of risk stratification in DCM is causing ongoing challenges in clinical practice (1, 2). Cardiovascular magnetic resonance (CMR) is regard as current gold standard for evaluating cardiac morphology and function. Assessment of myocardial deformation by CMR demonstrated increasing valuable potential than traditional parameters in predicting clinical outcomes (3, 4). Feature tracking (FT) has been established as a useful technique for identifying ventricular subtle systolic dysfunction and calculating myocardial strain (5-7). For atrial myocardial deformation, fast long-axis method showed stable reliability, and it also showed better reproducibility than FT method for obviating LA appendage and pulmonary veins (8). However, the interaction of biatrial and biventricular deformation capacity in patients with DCM is unclear. Therefore, the aim of this study was to evaluate prognostic value in DCM patients by analyzing biventricular global radial strain (GRS), global circumferential strain (GCS), and global longitudinal strain (GLS) through FT, as well as biatrial GLS through fast long-axis method.Methods
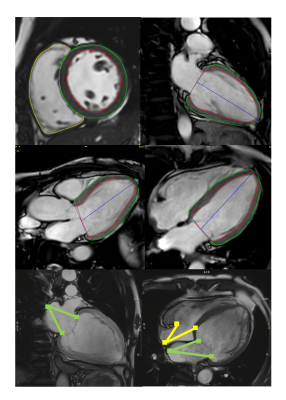
We retrospectively and consecutively enrolled participants who underwent CMR from September 2020 to May 2022. CMR examinations were performed and analyzed with 3.0-Tesla scanner (Ingenia CX, Philips Healthcare, the Netherlands) and CVI software (cvi42, Circle Cardiovascular Imaging Inc., Calgary, Alberta, Canada). FT and fast long-axis method were used to evaluate biventricular and biatrial myocardial strain parameters. Biventricular endocardial and epicardial borders, as well as biatrial atrioventricular junctions and midpoints of posterior atrial wall were tracked automatically with manual calibrations (Figure 1). DCM patients were stepwise divided into event group and no event group. Normally distributed continuous variables were compared by Student’s t-test. Non-normally distributed continuous variables were verified by Mann-Whitney U test. Categorical variables were assessed by chi-square test. Area under the curves (AUCs), specificity, sensitivity and optimal cut-off values were analyzed by receiver-operating characteristic (ROC) curve. All data were calculated by SPSS 26.0.0 (Inc., Chicago, IL, USA) or MedCalc (version 20, MedCalc Software, Ostend, Belgium). P < 0.05 was considered statistically significant.Results
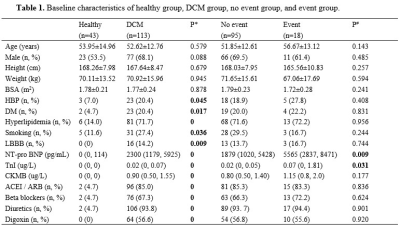
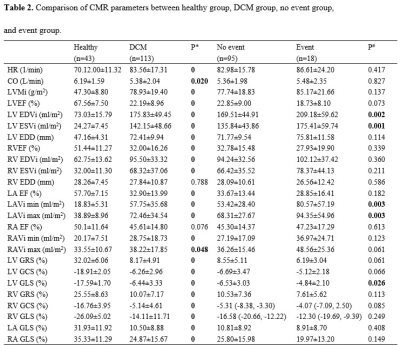
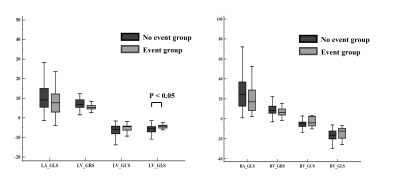
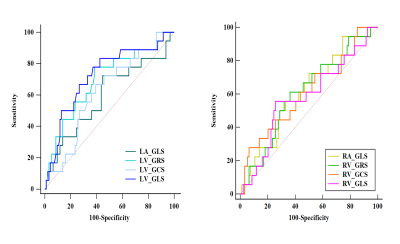
There were 113 DCM patients (52.62±12.76 years, 68.1% male) and 43 healthy volunteers (53.95±14.96 years, 53.5% male) finally recruited in this study. In comparison to healthy volunteers, DCM patients had higher prevalence of hypertension, diabetes mellitus, hyperlipidemia, smoking and left bundle branch block (all P < 0.05). DCM patients also showed higher levels in NT-proBNP, troponin I, CKMB, and more often received angiotensin converting enzyme inhibitor, beta blockers, diuretics, and digoxin. NT-pro BNP and TnI were obviously higher in event group relative to no event group (P < 0.05) (Table 1). DCM group also showed higher heart rate and left ventricular mass index, lower cardiac output, as well as lower biventricular ejection fraction and biatrial empty fraction, larger biventricular end-diastolic dimension, larger biventricular and biatrial volume index at end-diastolic and end-systolic stage (all P < 0.05). LV end-diastolic volume index and end-systolic volume index, as well as left atrial minimum and maximum volume index in event group were significantly larger than those in no event group (P< 0.05). Biventricular GRS, GCS, GLS, and biatrial GLS were significantly impaired in DCM group relative to control group. Furthermore, LV GLS was obviously impaired in event group than no event group (-4.84 ± 2.10% vs. -6.53 ± 3.03%, P < 0.05) (Table 2, Figure 2). In receiver-operating characteristic (ROC) analysis, LV GRS and GLS showed significant prognostic value in predicting MACEs with area under the curves of 0.696, 0.725 respectively (both P < 0.05) (Figure 3).Discussion
The reduction of biventricular GRS, GCS, GLS, and biatrial GLS were observed in DCM group in our findings, which was consistent with previous study about myocardial deformation characteristics (9). In the early stage of DCM, cardiac function can be modulated by the Frank-Starling law to increase myocardial contractility and compensate the reduced stroke volume(10). However, for the DCM patients who were at the end stage, decreased cardiac function was always associated with enlargement of ventricular chamber and decreased ventricular compliance (11). Reducing stroke volume of LV contributes to the increase of preload, then leading to LA dysfunction (12). With the interplay between LA and LV, pulmonary vascular pressure increases, further causing RV dysfunction (13). LV GLS showed significant prognostic value in predicting events occurrence in our result, GLS refers to systolic shortening of cardiac chamber in long-axis direction, which can be used to evaluate the motion ability of the ventricle in the cardiac cycle. And it stands for subendocardial dysfunction for evaluation (14). Anne et al. provided evidence that speckle tracking echocardiographic LV GLS emerged as an independent and incremental predictor of adverse outcome other than LVEF in patients with DCM (15). LV GLS was suggested to be routinely measured for DCM prognosis assessment.Conclusions
Biventricular global radial strain (GRS), global circumferential strain (GCS), global longitudinal strain (GLS), and biatrial GLS were significantly impaired in DCM group relative to control group. LV GLS was obviously impaired in event group than no event group, and it showed significantly prognostic value in predicting cardiovascular events. Comprehensive CMR examinations should be systematically performed, to improve the risk stratification and therapeutic management for patients with DCM.Acknowledgements
NoneReferences
1. Di Marco A, Brown P, Bradley J, Nucifora G, Claver E, de Frutos F, et al. Improved Risk Stratification for Ventricular Arrhythmias and Sudden Death in Patients With Nonischemic Dilated Cardiomyopathy. Journal of the American College of Cardiology. 2021;77(23):2890-905.
2. Gulati A, Jabbour A, Ismail T, Guha K, Khwaja J, Raza S, et al. Association of fibrosis with mortality and sudden cardiac death in patients with nonischemic dilated cardiomyopathy. JAMA. 2013;309(9):896-908.
3. Chirinos J, Sardana M, Ansari B, Satija V, Kuriakose D, Edelstein I, et al. Left Atrial Phasic Function by Cardiac Magnetic Resonance Feature Tracking Is a Strong Predictor of Incident Cardiovascular Events. Circulation Cardiovascular imaging. 2018;11(12):e007512.
4. Modin D, Biering-Sørensen S, Møgelvang R, Alhakak A, Jensen J, Biering-Sørensen T. Prognostic value of left atrial strain in predicting cardiovascular morbidity and mortality in the general population. European heart journal Cardiovascular Imaging. 2019;20(7):804-15.
5. Augustine D, Lewandowski A, Lazdam M, Rai A, Francis J, Myerson S, et al. Global and regional left ventricular myocardial deformation measures by magnetic resonance feature tracking in healthy volunteers: comparison with tagging and relevance of gender. Journal of cardiovascular magnetic resonance : official journal of the Society for Cardiovascular Magnetic Resonance. 2013;15:8.
6. Xu J, Yang W, Zhao S, Lu M. State-of-the-art myocardial strain by CMR feature tracking: clinical applications and future perspectives. European radiology. 2022.
7. Rajiah P, Kalisz K, Broncano J, Goerne H, Collins J, François C, et al. Myocardial Strain Evaluation with Cardiovascular MRI: Physics, Principles, and Clinical Applications. Radiographics : a review publication of the Radiological Society of North America, Inc. 2022;42(4):968-90.
8. Leng S, Tan R, Zhao X, Allen J, Koh A, Zhong L. Validation of a rapid semi-automated method to assess left atrial longitudinal phasic strains on cine cardiovascular magnetic resonance imaging. Journal of cardiovascular magnetic resonance : official journal of the Society for Cardiovascular Magnetic Resonance. 2018;20(1):71.
9. Popescu B, Beladan C, Calin A, Muraru D, Deleanu D, Rosca M, et al. Left ventricular remodelling and torsional dynamics in dilated cardiomyopathy: reversed apical rotation as a marker of disease severity. European journal of heart failure. 2009;11(10):945-51.
10. Weil J, Eschenhagen T, Hirt S, Magnussen O, Mittmann C, Remmers U, et al. Preserved Frank-Starling mechanism in human end stage heart failure. Cardiovascular research. 1998;37(2):541-8.
11. Długosz D, Surdacki A, Zawiślak B, Bartuś S, Chyrchel B. Impaired Left Ventricular Circumferential Midwall Systolic Performance Appears Linked to Depressed Preload, but Not Intrinsic Contractile Dysfunction or Excessive Afterload, in Paradoxical Low-Flow/Low-Gradient Severe Aortic Stenosis. Journal of clinical medicine. 2022;11(10).
12. Prioli A, Marino P, Lanzoni L, Zardini P. Increasing degrees of left ventricular filling impairment modulate left atrial function in humans. The American journal of cardiology. 1998;82(6):756-61.
13. Li Y, Xu Y, Tang S, Jiang X, Li W, Guo J, et al. Left Atrial Function Predicts Outcome in Dilated Cardiomyopathy: Fast Long-Axis Strain Analysis Derived from MRI. Radiology. 2022;302(1):72-81.
14. Ishizu T, Seo Y, Kameda Y, Kawamura R, Kimura T, Shimojo N, et al. Left ventricular strain and transmural distribution of structural remodeling in hypertensive heart disease. Hypertension (Dallas, Tex : 1979). 2014;63(3):500-6.
15. Raafs A, Boscutti A, Henkens M, van den Broek W, Verdonschot J, Weerts J, et al. Global Longitudinal Strain is Incremental to Left Ventricular Ejection Fraction for the Prediction of Outcome in Optimally Treated Dilated Cardiomyopathy Patients. Journal of the American Heart Association. 2022;11(6):e024505.
Figures