4857
High-resolution, free-breathing, fat-suppressed 3D Late Gadolinium Enhancement to define atrial wall scar after atrial fibrillation ablation
Rajesh Dash1,2, Henry Chubb3, Xianglun Mao4, Fara Nikbeh4, Pingni Wang4, Yuko Tada1, Gaspar Delso5, Martin Janich6, Sanjiv Narayan1, Daniel Ennis1, and Phillip C Yang1
1Stanford University, Stanford, CA, United States, 2Cardiovascular Institute, Stanford, CA, United States, 3Stanford Lucille Packard Childrens Hospital, Stanford, CA, United States, 4GE Healthcare, Inc., Menlo Park, CA, United States, 5GE Healthcare, Inc., Barcelona, Spain, 6GE Healthcare, Inc., Munich, Germany
1Stanford University, Stanford, CA, United States, 2Cardiovascular Institute, Stanford, CA, United States, 3Stanford Lucille Packard Childrens Hospital, Stanford, CA, United States, 4GE Healthcare, Inc., Menlo Park, CA, United States, 5GE Healthcare, Inc., Barcelona, Spain, 6GE Healthcare, Inc., Munich, Germany
Synopsis
Keywords: Myocardium, Arrhythmia, atrial fibrillation, ablation, atrial wall, scar, delayed gadolinium enhancement
Atrial fibrillation (AF) ablation procedures still face challenges to achieve durable restoration of sinus rhythm. Advanced cardiac MRI delayed enhancement can delineate atrial wall scar to aid in planning AF ablation. However, thin atrial walls demand more advanced sequence development. In this study, we report protocol optimizations for high-resolution, free-breathing, fat-suppressed 3D LGE to detect atrial wall scar. In three AF patients to date, we found progressive improvements in CNR and detailed the sequence modification that led to these improvements. Future iterations will be used to assess atrial scar in patients, pre- and post-AF ablation.INTRODUCTION
Atrial fibrillation (AF) ablation is a common treatment to reduce a patient’s AF burden. However, most patients require multiple ablations to achieve durable restoration of sinus rhythm. Cardiac MRI may detect atrial wall enhancement (Badger et al.; Gal et al.) and thereby inform/improve the success of AF ablation procedures. In this study, we report preliminary results of high-resolution, free-breathing, fat-suppressed 3D LGE to detect atrial wall scar. Specific sequence and protocol optimizations are described, with associated image and image analysis results to validate this imaging approach as a reliable, reproducible tool that may support AF ablation decision-making.METHODS
Three AF patients with prior ablation procedures were recruited for 3D LGE. A 3.0T SIGNA Premier MR system (GE HealthCare, Waukesha, WI) was used for all patient scans. The sequence employed is a free-breathing CMR scan with respiratory navigator, consisting of the following: SPGR readout with inversion recovery preparation, fat suppression, FOV 40x40cm2, 320x320x100, Slice Thickness=3.5mm, Inversion time (TI): 200-260ms; flip angle: 20 with fSPGR readout; Contrast agent Multihance; dose: 0.15mmol/kg (1.5x dose), acquisition timing: 15-25min after dose; TR/TE: 3.1/1.4ms 2.9ms/1.3ms (2nd and 3rd scans), Acceleration factor: 2 ARC, spatial resolution: 1.3x1.3x2.6mm (1st scan, 92 slices) to 1.3x1.3x3.5mm (2nd and 3rd scans, with 64 and 78 slices respectively), fat suppression, AIR Recon DL medium. Scan image quality was assessed using 2 independent readers evaluating the same image slice from each scan of the left atrial chamber, divided into 8 equal segments. Each segment was graded for: a) visualization of atrial wall continuity, using a scale of 100%/COMPLETE: 3, >50% MAJORITY: 2, <50% MINORITY: 1; and b) the presence of scar in each segment: 0 - ABSENT, 1 - PRESENT. Inter-observer variability was then calculated. Average contrast-to-noise ratio (CNR) measurements were also made using multiple regions of interest along areas of identified left atrial myocardial scar compared to left atrial lumen blood pool.RESULTS
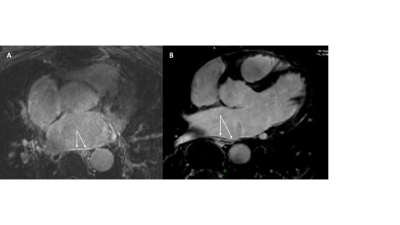
Delayed enhancement of the left atrial wall was noted on all three patient scans, with notable improvements in scar identification qualitatively and image quality quantitatively. Image quality and scar identification was scored qualitatively by two independent observers for atrial wall continuity and scar absence or presence across 8 segments. Inter-observer agreement overall across studies was high (72% for atrial wall continuity, 87.5% for scar presence) for each segment's image quality and for the presence absence of scar), but there was no significant difference between studies in observer scoring. Additional observer data is pending collection and will be incorporated. Scar CNR compared to blood pool was measured for each AF patient (CNR of identified scar from 1st patient scan: 5.9+/-0.9; 2nd patient scan: 6+/-3.5; 3rd patient scan: 15.2 +/-8.2). Scan sequence adjustments were made to spatial resolution, and TR/TE parameters to improve the sequence performance. See Figure 1A,B.DISCUSSION/CONCLUSION
While 3D LGE can successfully detect detailed atrial wall enhancement in AF patients post-ablation, ongoing protocol improvements are needed in both pre- and post-AF ablation patients to achieve a robust and reproducible high quality imaging of the atrial wall.Acknowledgements
GE Healthcare, Inc. for in-kind support of this research
Cardiovascular Institute, Stanford University
NIH/NHLBI: PY; DOD: PY
References
Pim Gal and Nassir F. Marrouche. Magnetic resonance imaging of atrial fibrosis: redefining atrial fibrillation to a syndrome. European Heart Journal (2017) 38, 14–19.
Badger et al. Evaluation of Left Atrial Lesions After Initial and Repeat Atrial Fibrillation AblationLessons Learned From Delayed-Enhancement MRI in Repeat Ablation Procedures. Circulation: Arrhythmia and Electrophysiology. 2010;3:249–259.
DOI: https://doi.org/10.58530/2023/4857