4841
Strain may reflect cardiac segments with high coronary artery calcium score and the risk of myocadiac ischemia1Department of Radiology, Renmin Hospital of Wuhan University, Wuhan, China, 2GE Healthcare, MR Research China, Beijing, China, 3GE Healthcare, Beijing, China
Synopsis
Keywords: Myocardium, Ischemia, strain
Preclinical disease is primarily assessed through the coronary artery calcium score (CACS) and used for risk assessment. Our study demonstrated that the moderate correlation of the CACS and strain, suggesting atrial or ventricular myocardium and vascular changes influence each other. In addition, there were statistically different strain values between CAD and non-CAD patients. Strain analysis for cine CMR can add functional information such as chamber wall movement on early prediction of myocardium abnormities like myocadiac ischemia and be beneficial to patients who receive one-stop check-ups for less imaging time, no contrast, and radiation-free screening.Purpose
Chest pain is one common symptom of coronary artery disease (CAD), but some patients have atypical symptoms to be identified accurately in time [1,2]. Coronary artery calcium scoring (CACS) is a strong independent predictor of cardiovascular events and used to screen the requirement for cardiac perfusion exam [3]. Time-saving artificial intelligence (AI)-based CACS is well correlated with manual CACS in terms of risk categories [4-6]. Myocardial strain analysis shows changes in cardiac function, ventricular wall motion, and chamber mechanics as well as elevates the accuracy of diagnosis, it reflects the contraction of myocardial fibers in different directions; the radial strain (RS) is perpendicular to the epicardium towards the center of the cavity, the circumferential strain (CS) is tangential to the epicardial wall in the circumferential direction and the longitudinal strain (LS) is tangential to the myocardial wall along the long axis of the cavity [7]. The aim of this study was to investigate the diagnostic value of strain parameters in assessment myocardium function and the performance on differentiating patients with atypical symptoms CAD from patients with acute chest pain.Materials and Methods
This study was approved by our hospital (Approval No. 2022K-K083). A total of 40 acute chest pain (include 20 CAD patients and 20 patients without CAD) underwent cardiovascular magnetic resonance (CMR) scans, including 4-chamber (4CH) FIESTA Cine,long-axis (LA) FIESTA Cine,short axis (SA) FIESTA Cine,left ventricle outflow tract (LVOT) FIESTA Cine on 3.0 T MRI scanner (Signa Architect, GE Healthcare) at our hospital from April to September 2022. Parameters of all cine scans were shown in Table 1.All CMR-Cine sequences were analyzed in cvi42 software (Circle Cardiovascular Imaging, Calgary, Canada) to compute left ventricle global CS (LVGCS), LVGRS, LVGLS, right ventricle GCS (RVGCS), RVGRS,RVGLS, left atrium long-axis strain (LALAS), right atrium long-axis strain (RALAS) (Fig.1.). All analysis were performed by two radiologists with more than 5 years of experience in the diagnosis of cardiovascular diseases without knowing patient's condition. One of the radiologists re-evaluated the strain values after 1 month.
All patients underwent a non-enhanced chest CT scan 1 day prior to the CMR examination (Xtream Edition, GE Healthcare, 256Rows). The Agatston score for left anterior descending coronary artery (LAD-Agatston), left circumflex coronary artery (LCX-Agatston) and right coronary artery (RCA-Agatston) and a sum score of abovementioned arteries (total-Agatston) of the non-gated chest CT flat-scan was obtained using the AI-CACS software from Shukun Technology.
Intra- and inter-observer agreements on each measurement were examined using intra-correlation coefficient (ICC). Pearson correlation analysis for the correlation between the strain value and the Agatston score of the CACS was conducted using SPSS (version 25.0, Chicago, IL). Independent sample t test or Mann-Whitney t test were used to compare group difference depending on data normality and equality of variance. P<0.05 was considered statistical difference.
Results
Both intra- and interobserver agreements on strain were good (ICC = 0.80 (0.63,0.90), 0.78 (0.58,0.88), all p < 0.001). The differences of LVGLS, RVGLS and RALAS between the CHD group and the non-CHD group were statistically significant (t LVGLS=-4.43, t RVGLS=-2.78, Z RALAS=-2.71, all p < 0.05) (Fig. 2).Total Agatston score, LAD Agatston score, LCX Agatston score and RCA Agatston score was 97.23, 8.45, 42.08, 0.98, respectively (Fig. 3). CACS, including Total-Agaston, LAD-Agaston, LCX-Agaston, and RCA-Agaston, were correlated with strain parameters (p < 0.05) (Table 2).
Discussion and conclusions
Our study with good intra and inter-observer consistency presented significant correlation of strain and Agaston score, suggesting strain analysis may assist to early diagnose overall morphological structure and calcification-induced alterations of myocardium systolic function including hemodynamics and biomechanics of dynamic deformation [4,8]. CAC affects endothelial function, vasodilation and luminal blood flow through various mechanisms, in turn altering peripheral myocardial blood supply and function [9-12]. Vascular calcification is highly correlated with cardiovascular disease mortality. Intimal calcification, endothelial cell injury, increased expression of molecules such as cell adhesion are all associated with atherosclerosis, while intimal calcification is a non-occlusive process that leads to increased vascular stiffness and reduced vascular compliance, and arterial stiffness is a hallmark of structural and functional changes in the vessel wall, ultimately leading to organ damage [13].In this study, CACS was correlated with GCS, GRS, GLS, RALAS. The GLS and RALAS between the CAD group and the non-CAD group were statistically significant, suggesting vascular mechanical alternations possibly ahead of blood perfusion gave an early warning of ischemic myocardium. GLS or GCS is a predictor of negative left ventricular remodeling after myocardial infarction and can be an early predictor of poor prognosis such as heart failure due to left ventricular dysfunction, and GCS can reveal mildly reduced left ventricular systolic function due to the pathological process of infarction while GAS has potential in risk stratification for myocardial infarction. Strain analysis quantitatively reflects local and global LV function and is more sensitive than LV ejection fraction value and visual assessment of ventricular wall motion [14,15]. To sum up, CMR myocardial strain technique can fill the gap of conventional CMR in local myocardial assessment such as myocardial motion and functional abnormalities in different axis of hearts directions, and has important potential value in accurate diagnosis and prognostic assessment.
Acknowledgements
No acknowledgement found.References
[1] Broncano J, Bhalla S, Caro P, et al. Cardiac MRI in patients with acute chest pain. Radiographics,2021,41(1):8-31. PMID: 33337967.
[2] Dastidar AG, Baritussio A, De Garate E, et al. Prognostic role of CMR and conventional risk factors in myocardial infarction with nonobstructed coronary arteries. JACC Cardiovasc Imaging, 2019,12(10):1973–1982. DOI: 10.1016/j.jcmg.2018.12.023.
[3] Min Jae Cha, Sung Mok Kim, Yiseul Kim, et al. Unrecognized myocardial infarction detected on cardiac magnetic resonance imaging: Association with coronary artery calcium score and cardiovascular risk prediction scores in asymptomatic Asian cohort. PLoS One, 2018,13(9): e0204040. DOI: 10.1371/journal.pone.0204040. eCollection 2018.
[4] Rijlaarsdam-Hermsen D, Lo-Kioeng-Shioe M, van Domburg RT, et al. Stress-Only Adenosine CMR Improves Diagnostic Yield in Stable Symptomatic Patients with Coronary Artery Calcium. JACC Cardiovasc Imaging, 2020,13(5):1152-1160. DOI: 10.1016/j.jcmg.2019.12.009.
[5] Bavishi C, Argulian E, Chatterjee S, Rozanski A. CACS and the frequency of stress-induced myocardial ischemia during MPI: a meta-analysis. J Am Coll Cardiol Img, 2016,9(5):580–589. DOI:10.1016/j.jcmg.2015.11.023.
[6] Xu J, Liu J, Guo N, et al. Performance of artificial intelligence-based coronary artery calcium scoring in non-gated chest CT. Eur Radiol, 2021,145(12):1-11. DOI: 10.1016/j.ejrad.2021.110034.
[7] Shiqin Yu, Shihua Zhao. The application of cardiac MR strain analysis in myocardial infarction. Chinese Journal of Radiology, 2020,54(12): 1224-1228. DOI: 10.3760/cma.j.cn112149-20200307-00337.
[8] Arthur E. Stillman, Matthijs Oudkerk, David A. Bluemke, et al. Imaging the myocardial ischemic cascade. The International Journal of Cardiovascular Imaging, 2018,34(1):1249–1263. DOI:10.1007/s10554-018-1330-4.
[9] Coenen A, Rossi A, Lubbers MM, et al. Integrating CT myocardial perfusion and CT-FFR in the work-up of coro nary artery disease. JACC-Cardiovasc Imag, 2017, 10(7):760-770. DOI:10.1016/j.jcmg.2016.09.028.
[10] Shah SV, Shukla AM, Bose C, et al. Recent Advances in Understanding the Pathogenesis of Atherosclerosis in CKD Patients. J Ren Nutr,2015,25(2):1-4. DOI:10.1053/j.jrn.2014.10.024.
[11] Wilson S, Mone P, Jankauskas SS, et al. Chronic kidney disease: Definition, updated epidemiology, staging, and mechanisms of increased cardiovascular risk. J Clin Hypertens (Greenwich),2021,23(4):1-4. DOI:10.1111/jch.14186.
[12] Nadine Kaesler, Anne Babler, Jürgen Floege, et al. Cardiac Remodeling in Chronic Kidney Disease. Toxins, 2020, 12(3): 1-16. DOI: 10.3390/toxins12030161.
[13] Ishiura J, Nakamori S, Ishida M, et al. Serial native T1 assessment for LV functional recovery in recent-onset DCM: a comparison with histology. JACC Cardiovasc Imaging. 2022,15(2):1-11. DOI: 10.1016/j.jcmg.2021.08.008.
[14] Xinru Guo, Yisha Li, Ying Yang, et al. Noninvasive markers of arterial stiffness and renal outcomes in patients with chronic kidney disease. J Clin Hypertens. 2021,23(1):823–830. DOI: 10.1111/jch.14185.
[15] Palaskas N, Lopez-Mattei J, Durand JB, et al. Immune Checkpoint Inhibitor Myocarditis: Pathophysiological Characteristics, Diagnosis, and Treatment. J Am Heart Assoc, 2020,9(2): e013757. DOI: 10.1161/JAHA.119.013757.
Figures
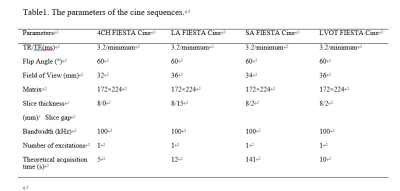
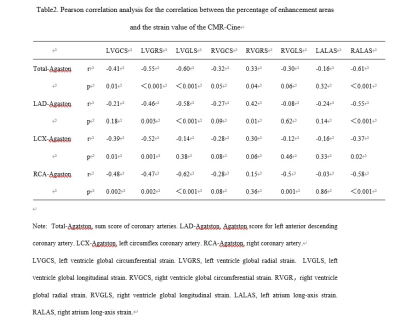
Table2. Pearson correlation analysis for the correlation between the percentage of enhancement areas and the strain value of the CMR-Cine
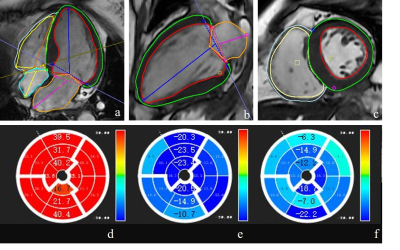
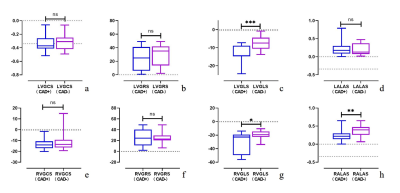
Figure 2. The differences of LVGCS(a), LVGRS(b), LVGLS(c), LALAS(d), RVGCS(e), RVGRS(f), RVGLS(g), RALAS(h) between the CAD group and the non-CAD group. The differences of LVGLS, RVGLS and RALAS between the CAD group and the non-CAD group were statistically significant (t LVGLS=-4.43, t RVGLS=-2.78, Z RALAS=-2.71, all p < 0.05).
Note:LV, left ventricle. RV, right ventricle. GCS, global circumferential strain. GRS, global radial strain. GLS, global longitudinal strain. LALAS, left atrium long-axis strain. RALAS, right atrium long-axis strain.

Figure 3 The Agaston of the CACS for all patients. Total Agatston score, LAD Agatston score, LCX Agatston score and RCA Agatston score was 97.23, 8.45, 42.08, 0.98, respectively.
Note: CACS, coronary artery calcification score.