4834
Based on cardiovascular magnetic resonance imaging for predicting right ventricular dysfunction in STEMI patients by Machine learning1Department of Radiology, The First Medical Center of PLA General Hospital, Beijing, China, 2Philips Healthcare(Beijing), Beijing, China
Synopsis
Keywords: Heart, Heart, right ventricular dysfunction; machine learning techniques; ST-Segment-Elevation myocardial infarction
In clinical work, right ventricular (RV) dysfunction has been ignored in acute ST-Segment-Elevation myocardial infarction (STEMI) patients. And previous studies have shown the interaction between left ventricular (LV) and RV. The aim of this study was to assess RV function by cardiovascular magnetic resonance feature tracking (CMR-FT) and to explore what factors affect RV dysfunction by machine learning techniques. The results showed that the incidence of RV dysfunction was 32.28% in STEMI patients and the occurrence of RV dysfunction was associated with RV end-systolic volume index, LV ejection fraction (EF), and interventricular septum radial strain by machine learning technique.Introduction
The left ventricular (LV) function had considerable achievements in risk assessment over the last decades in acute ST-Segment-Elevation myocardial infarction (STEMI) patients1,2, while the right ventricular (RV) function is difficult to evaluate due to its complex anatomical structure, so it is often disregarded. Cardiovascular magnetic resonance feature tracking (CMR-FT), as a newer technique, can provide a comprehensive assessment of cardiac morphology, function, and tissue characterization, to accurately detect RV dysfunction. The animals study have found that there is a certain correlation between the LV and RV from the anatomical perspective, and even the interventricular septum (IVS) bears a very large part of the systolic function of the RV, but lack of quantitative research3. So, the present study aimed to assess RV function and develop a prediction model to explore the predictive value of clinical parameters, the structure, and function of LV and IVS for RV dysfunction by using machine learning techniques in STEMI patients.Methods
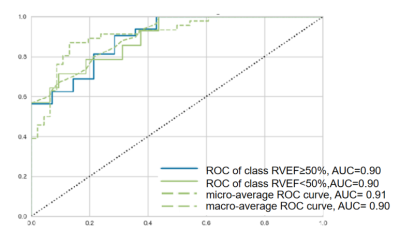
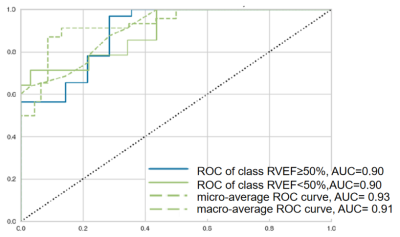
189 consecutive STEMI patients who underwent successful percutaneous coronary intervention were enrolled. All subjects underwent CMR with late gadolinium enhancement imaging (LGE) and cine images on a 1.5T scanner (Multiva, Philips Healthcare, Netherlands). The short-axis LGE images was used for visualizing scar of LV and RV, and to calculate infarction size of LV by using the full-width-at-half maximum method[4]. The End-diastolic volume index (EDVI), end-systolic volume index,(ESVI), ejection fraction (EF), average wall thickening rate (WTR) and radial strain (RS) of RV, LV, and interventricular septum (IVS) were measured by CMR-FT from cine images. The RVEF=50% was used as the cutoff value to divide patients into reduced RVEF or non-reduced groups. Univariate logistic regression analysis was used to determine independent predictors of RV dysfunction in CMR-FT and clinical parameters. Based on this univariate analysis, covariates (P <0.05) were selected for further machine learning techniques. There are totally 17 kinds of machine learning classification models that were tested using ISMI (Philips), including Logistic Regression, Decision Tree, Gradient Boosting Classifier, Ada Boost Classifier, Linear Discriminant Analysis, Extra Trees Classifier.etc.Then, the STEMI patients were randomly divided into 151 cases for training sets and 38 cases for an independent testing cohort at a ratio of 8:2. The pipeline will calculate the training set and evaluates the performance of all classifier by using 10-fold cross-validation, then choose the best performance model to create the training model .Receiver operating characteristic (ROC) curves were drawn, and the areas under the curve (AUC) were calculated to evaluate the diagnostic efficiency of the models in distinguishing RV dysfunction.Results
Among the 189 patients, the incidence of reduced RVEF was 32.28% (61/189). In 61 patients With reduced RVEF, 36(59%) infarct-related artery was right coronary artery (RCA). As shown in Table 1, the patients with reduced RVEF presented with significantly lower LVEF, LV RS and IVS average wall thickening rate and greater LV infarct size compared with the non- reduced RVEF group. Patients with reduced RVEF also presented with a significantly higher RV ESVI and a lower RV RS. Table 2 shows the univariable logistics regression analyses for the reduced RVEF. Based on this univariable analysis, The clinical parameters (gender, Drinking, and the culprit lesion in the RCA.ect.) and the CMR parameters (LV ESVI, LVEF , LV RS , LV infarct size, IVS RS, RV ESVI, and presence of RV infarction, etc.) were selected for further machine learning techniques. For the machine learning model, the classifier of Gradient Boosting Classifier (Figure 1) and Linear Discriminant Analysis (Figure 2) yielded an AUC of 0.84 and 0.85 in the training set, respectively. In the testing set, the accuracy of the Gradient Boosting Classifier and Linear Discriminant Analysis was 0.84 and 0.82, respectively. Of these two classifiers, RV ESVI, LVEF, and IVS RS were the most important features.Discussion
In clinical practices, we always ignore RV dysfunction in STEMI patients. However, our study showed that the incidence of RV dysfunction was 32.28%, accounting for a large proportion of STEMI patients. Previous anatomical studies have shown that there is an interactive relationship between RV and LV shape and function, meaning that changes in one ventricle can affect the other 4,5. Our experiments have further found that LVEF and IVS RS were correlated with RV dysfunction in a predictive model by machine learning models. There is consistent with previous studies that there is an interaction between LV and RV.Conclusion
CMR-FT provides a reliable method for evaluating right ventricular function. In this study, RV dysfunction was detected in 32.28% of STEMI patients. In addition, a machine learning model based on clinical and CMR parameters was built for predicting RV dysfunction. We found that the occurrence of RV dysfunction was not only related to RV ESVI but also affected by the function of the LV and IVS.Acknowledgements
No acknowledgement found.References
1. Ibanez B, James S, Agewall S, Antunes MJ, Bucciarelli-Ducci C, Bueno H, et al. 2017 ESC Guidelines for the management of acute myocardial infarction in patients presenting with ST-segment elevation: The Task Force for the management of acute myocardial infarction in patients presenting with ST-segment elevation of the European Society of Cardiology (ESC). Eur Heart J. 2018;39:119-77.
2. Reindl M, Tiller C, Holzknecht M, Lechner I, Eisner D, Riepl L, et al. Global longitudinal strain by feature tracking for optimized prediction of adverse remodeling after ST-elevation myocardial infarction. Clin Res Cardiol. 2021;110:61-71.
3. Apitz C, Honjo O, Humpl T, Li J, Assad RS, Cho MY, et al. Biventricular structural and functional responses to aortic constriction in a rabbit model of chronic right ventricular pressure overload. J Thorac Cardiovasc Surg. 2012;144:1494-501.
4. Mauger C, Gilbert K, Lee AM, Sanghvi MM, Aung N, Fung K, et al. Right ventricular shape and function: cardiovascular magnetic resonance reference morphology and biventricular risk factor morphometrics in UK Biobank. J Cardiovasc Magn Reson. 2019;21:41.
5. Elzinga G, Piene H, de Jong JP. Left and right ventricular pump function and consequences of having two pumps in one heart. A study on the isolated cat heart. Circ Res. 1980;46:564-74.
Figures

Table 1 CMR features of the study population
CMR, cardiovascular magnetic resonance; RVEF, right ventricular ejection fraction; LVEF, left ventricular ejection fraction; LV, left ventricular, RV, right ventricular; EDVI, end-diastolic volume index; ESVI, end-systolic volume index; RS, radial peak strain; WTR, wall thickening rate; MVO, microvascular obstruction; IVS, interventricular septum
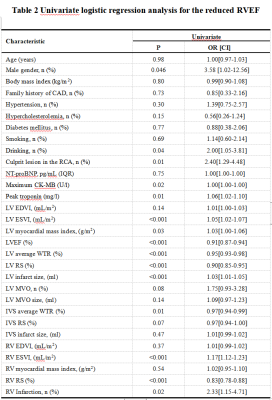
Table 2 Univariate logistic regression analysis for the reduced RVEF
CAD, coronary artery disease; RCA, right coronary artery; NT-proBNP, N-terminal pro b-type natriuretic peptide; CK-MB, creatine kinease MB; LV, left ventricular, RV, right ventricular; EDVI, end-diastolic volume index; ESVI, end-systolic volume index; RS, radial peak strain; WTR, wall thickening rate; MVO, microvascular obstruction; IVS, interventricular septum