4833
Delays in first medical contact to primary interventional therapy and left ventricular remodeling in myocardial infarction
Jiali Wang1, Kai Xu1, Chunfeng Hu1, Yankai Meng1, Shuguang Han1, Yuan Lu1, Peng Wu2, Lu Han2, and Yongzhou Xu3
1The Affiliated Hospital of Xuzhou Medical University, Xuzhou, China, 2Philips Healthcare, Shanghai, China, 3Philips Healthcare, Guangzhou, China
1The Affiliated Hospital of Xuzhou Medical University, Xuzhou, China, 2Philips Healthcare, Shanghai, China, 3Philips Healthcare, Guangzhou, China
Synopsis
Keywords: Myocardium, Ischemia
Early reperfusion and early evaluation of cardiac adverse left ventricular remodeling (ALVR) have become important aspects of treatment for ST-segment elevation myocardial infarction (STEMI) post-percutaneous coronary intervention (PCI). The aim of this study was to investigate the predictive value of emergency medical service (EMS) delays on the severity of myocardial injury in STEMI patients after PCI. Cardiac magnetic resonance (CMR) cine, myocardial strain, and scar characteristics were analyzed. The first medical contact to balloon (FMC2B) time was recorded. FMC2B time > 90 min led to poor recovery of cardiac function and was an independent predictor of ALVR.Introduction
A considerable proportion of patients with ST-segment elevation myocardial infarction (STEMI) suffer adverse left ventricular remodeling (ALVR) after primary percutaneous coronary intervention (PCI), leading to adverse cardiovascular events. Early evaluation of ALVR has become an important aspect of STEMI treatment 1-2. The first medical contact to balloon (FMC2B) time is an important time point that impacts the care process of STEMI patients. Cardiac magnetic resonance (CMR) imaging can be used to show the anatomy of the cardiac structure, myocardial function, and infarction characteristics, including myocardial infarct size (IS) and microvascular obstruction (MVO)3-4. Therefore, the primary purpose of this study was to investigate the relationship between FMC2B delays, and short-term ALVR in STEMI patients post-PCI. The secondary purpose was to investigate the relationship between FMC2B delays and the recovery of cardiac function using CMR to provide clinicians with strategies for decision-making during the early evaluation of the condition of STEMI patients and for the prevention of serious adverse events.Methods
This was a retrospective analysis of STEMI patients who received emergency PPCI treatment and two CMR examinations 7 days (acute phase) and 3-4 months (convalescent phase) after PPCI in our hospital. Patients with multiple vessel diseases and patients with a previous history of myocardial infarction were excluded (Figure 1). CMR scans were performed on a 3.0T all-digital MR scanner (Ingenia, Philips Healthcare, Amsterdam, Netherlands) with a surface body coil and posterior spinal coil. The protocols included steady-state free precession (SSFP), T2-weighted, and LGE. The SSFP image was obtained with 30 phases in the cardiac cycle, whose parameters were as follows: field of view 350*350 mm; repetition time/echo time (TR/TE), 2.6/1.3 ms; flip angle 45°, and slice thickness 8 mm. The LGE image was obtained 10–15 min after the administration of contrast agents. The parameters were as follows: TR/TE 3.0/6.1 ms, flip angle 25° , slice thickness 8 mm. CMR analyses were performed using a commercially available workstation (Circle Cardiovascular Imaging, cvi42®, v5.12.4, Calgary, Alberta, Canada). Left ventricular end-diastolic volume (LVEDV), left ventricular end-systolic volume (LVESV), and left ventricular ejection fraction (LVEF) and CMR feature-tracking (FT) strain analysis were obtained from the short-axis cine-CMR sequence. The IS and MVO were evaluated by the LGE images5. The LVEDV and LVESV parameters from two CMR examinations were used to categorize STEMI patients into three groups6: Group 1: reverse LV remodeling: an LVESV decrease ≥ 12%; Group 2: no LV remodeling: the changes in the LVEDV and LVESV were < 12%; and Group 3: adverse LV remodeling: an LVEDV increase ≥ 12%. Statistical analysis was performed using the statistical software SPSS 22.0.Results
1. Patients with ALVR had higher levels of high-sensitivity cardiac troponin-T (hs-cTnT) and creatine kinase-myocardial band (CK-MB), longer FMC2B times, larger IS, larger MVO, and a lower LVEF in the acute phase.2. In patients who experienced EMS delays, the IS and MVO were larger and the recovery of LVEF and global longitudinal strain (GLS) were worse (Table 1). Case examples of CMR are shown in Figure 2.
3. FMC2B time > 90 min and IS were found to be independent factors influencing ALVR in STEMI after PCI. In patients with an EMS delay, the incidence of ALVR after PCI was approximately 2.7 times higher than that of the patients with an FMC2B time ≤ 90 min (p=0.028, OR=2.661 95% CI 1.112-6.367) (Table 2).
Discussion
The CHINA Patient-Centered Evaluative Assessment of Cardiac Events (China PEACE) showed that delayed treatment of STEMI led to a prolonged total ischemic time and the proportion of patients with early reperfusion treatment was relatively low in China7. Most previous studies focused only on the diagnostic value of CMR, and the time to myocardial ischemia was not included in these studies. In the current study, an FMC2B time > 90 min was a predictor of ALVR in STEMI patients even after adjustment for IS. Therefore, more attention should be given to reducing the FMC2B time and the total time of myocardial ischemia. Delays in FMC2B may be due to delays in medical decision-making procedures; a patient being admitted to the hospital on their own rather than through an ambulance; and waiting times for screening tests, such as nucleic acid tests, particularly between January 2020 and March 2020, when the COVID-19 pandemic was at its peak8.Myocardial strain parameters provided by CMR-FT can provide additive value to current imaging diagnostics, especially for those with severe renal impairment9. The GLS improved in all patients at the 4-month follow-up after reperfusion in our study, while the no-EMS delay group showed better recovery than the EMS delay group, which may suggest that EMS delays lead to more severe infarct-related myocardial injury. Larger studies will be required to determine whether CMR myocardial strain can be a promising parameter for early risk stratification after reperfusion in STEMI patients. In conclusion, EMS delays were associated with poor recovery of cardiac function and short-term adverse LV remodeling.
Conclusion
To summarize, FMC2B time >90 min was associated with poor recovery of cardiac function and short-term adverse LV remodelingAcknowledgements
No acknowledgement found.References
- O Gara PT, Kushner FG, Ascheim DD, et al. 2013 ACCF/AHA Guideline for the management of ST-Elevation Myocardial Infarction. Circulation, 2013, 127(4): e362-425.
- Ibanez B, James S, Agewall S, et al. 2017 ESC Guidelines for the management of acute myocardial infarction in patients presenting with ST-segment elevation. Eur. Heart J, 2018, 39(2): 119-177.
- Pezel T, des Horts TB, Schaaf M, et al. Predictive value of early cardiac magnetic resonance imaging functional and geometric indexes for adverse left ventricular remodeling in patients with anterior ST-segment elevation myocardial infarction: A report from the CIRCUS study. Arch Cardiovasc Dis, 2020, 113(11):710-720.
- Ibanez B, Aletras AH, Arai AE, et al. Cardiac MRI Endpoints in Myocardial Infarction Experimental and Clinical Trials: JACC Scientific Expert Panel. J Am Coll Cardiol. 2019, 74(2):238-256.
- Yu SQ, Zhou JY, Yang K, et al. Correlation of myocardial strain and late gadolinium enhancement by cardiac magnetic resonance after a first anterior ST-segment elevation myocardial infarction. Front Cardiovasc Med, 2021, 8: 705487.
- Bulluck H, Carberry J, Carrick D, et al. Redefining adverse and reverse left ventricular remodeling by cardiovascular magnetic resonance following ST-segment-elevation myocardial infarction and their implications on long-term prognosis. Circ Cardiovasc Imaging, 2020, 13(7): e009937.
- Li J, Li X, Wang Q, et al. ST-segment elevation myocardial infarction in China from 2001 to 2011 (the China PEACE-Retrospective Acute Myocardial Infarction Study): a retrospective analysis of hospital data. Lancet, 2015, 385(9966): 441-451.
- Hauguel-Moreau M, Pillière R, Prati G, et al. Impact of Coronavirus Disease 2019 outbreak on acute coronary syndrome admissions: four weeks to reverse the trend. J Thromb Thrombolysis. 2021, 51(1):31-32.
- Reindl M, Tiller C, Holzknecht M, et al. Global longitudinal strain by feature tracking for optimized prediction of adverse remodeling after ST-elevation myocardial infarction. Clin Res Cardiol. 2021, 110:61-71.
Figures
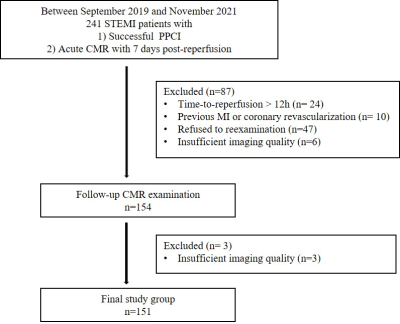
Figure 1 Patient flowchart.
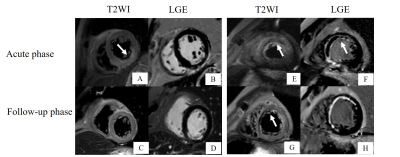
Figure 2. Representative
CMR images of two patients with STEMI. Patient 1 (A–D) A 70-year-old female,
FMC2B time = 53 min. Inferior myocardial oedema (A) and subendocardial
myocardial infarction(B) in acute CMR demonstrated were slightly reduced in
follow-up (C-D). Patient 2 (E-H) A 42-year-old male. FMC2B time = 135 min.
Anterior wall and septum myocardial infarction(E-F) in acute CMR, and cardiac
scarring had formed (G, H) in the follow-up.
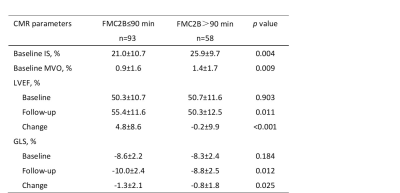
Table 1 Comparison and change in the CMR parameters between the different treatment
time groups
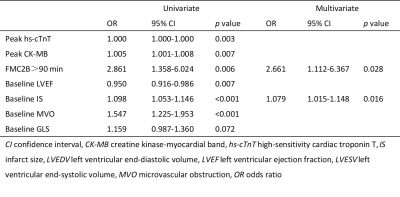
Table 2 Logistic
regression analysis for the prediction of short-term adverse LV remodeling
DOI: https://doi.org/10.58530/2023/4833