4830
Predictive value of total ischemic time and T1 mapping after emergency PCI in acute ST-segment elevation myocardial infarction1The Affiliated Hospital of Xuzhou Medical University, Xuzhou, China, 2Philips Healthcare, Shanghai, China, 3Philips Healthcare, Guangzhou, China
Synopsis
Keywords: Myocardium, Ischemia, T1 mapping
ST-segment elevation myocardial infarction (STEMI) remains a major cause of morbidity and mortality worldwide, effective risk stratification is crucial for the management of STEMI. This study sought to investigate the predictive value of total ischemic time (symptom onset to balloon, S2B), native T1 and extracellular volume (ECV) in STEMI patients undergoing primary percutaneous coronary intervention (PCI). We found regardless of microvascular obstruction (MVO) or not, ECV in myocardial infarction (ECVMI) was significantly correlated with S2B time, while native T1 was not. In the 4-month follow-up, ECVMI was independently associated with final larger infarct size in multivariable regression analysis.Introduction
In ST-segment elevation myocardial infarction (STEMI), the benefits of primary percutaneous coronary intervention (PCI) could be maximized if angioplasty is performed within symptom-to-balloon (S2B) time < 2 hours, it helps decrease mortality rates1. Cardiac magnetic resonance (CMR) T1-mapping quantitatively measures the myocardial T1 relaxation time, native and post-contrast T1 mapping allows for the estimation of myocardial extracellular volume (ECV)2. At present, there is less research on the influence of S2B time on native T1 and ECV values, as well as the combined predictive effect of S2B time and T1 mapping following emergency PCI. Therefore, we sought to assess the relationship between ischemic time and native T1 and ECV values. In addition, we examined the impact of ischemic time and T1 mapping on infarct characteristics, which may provide prospective useful information for predicting myocardial injury in STEMI patients.Methods
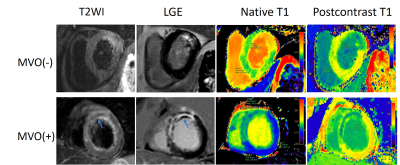
127 STEMI patients who received emergency primary PCI remained in the study and 61 of them completed the convalescent phase CMR examination. According to the S2B time, patients were divided into 3 groups: S2B time < 120 min (group 1), 120-300 min (group 2), >300 min (group 3). CMR scans were performed on a 3.0T MR scanner (Ingenia, Philips Healthcare, Best, The Netherlands), using the surface body coil and the posterior spinal coil. CMR protocol included cine, native T1 mapping, post-contrast T1 mapping, and late gadolinium enhancement (LGE). The parameters were as follows: field of view, 350*350 mm; repetition time/echo time (TR/TE), 2.6/1.3 ms; flip angle, 45°; and slice thickness, 8 mm. The LGE-CMR parameters were as follows: TR/TE, 3.0/6.1 ms; flip angle, 25°; and slice thickness, 8 mm. T1 mapping was scanned using modified Look-Locker inversion recovery (MOLLI) with a 5 s (3 s) 3 s scan scheme covering the base, mid-ventricular, and apex levels of LV. CMR analysis were performed using a commercially available workstation (Circle Cardiovascular Imaging, cvi42®, v5.12.4, Calgary, Alberta, Canada)3. T1 mapping images automatically generated by the MR scanner were exported to the dedicated workstation (Intelligence Space Portal, version 10.1, Philips Healthcare, Best, The Netherlands) for further analysis. All statistical analyses were performed with SPSS (version 23.0, IBM Corporation, Armonk, NY, USA), and p<0.05 was considered statistically significant.Results
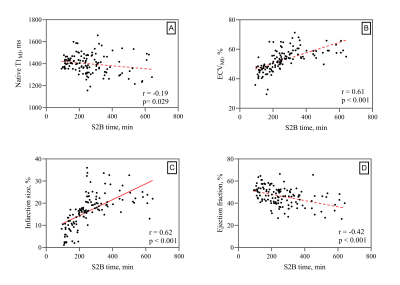
1. Patients with extended ischemic time suffer larger infarct size (IS), lower left ventricular ejection fraction (LVEF) and higher ratios of MVO (+).2. S2B time correlated with ECV in myocardial infarction (ECVMI), IS and LVEF, while no significant correlations with native T1 in MI (T1MI) (Fig 1).
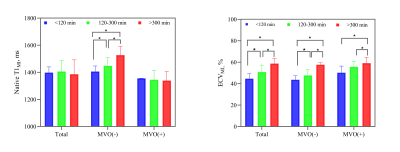
3. In all subjects and MVO (+) subgroup, native T1MI did not differ among the three ischemic time groups, while in MVO (-) subgroup, native T1MI increased with the prolonged S2B time.
4. ECVMI was significantly greater in group 3 than in the other two groups no matter whether MVO was present or not (Fig. 2, Fig. 3).
5. In all 61 subjects who completed the second CMR examination during the follow-up period, IS, LVEF and native T1MI all improved from baseline to 4 months follow-up. Group 1 had the smallest change in IS.
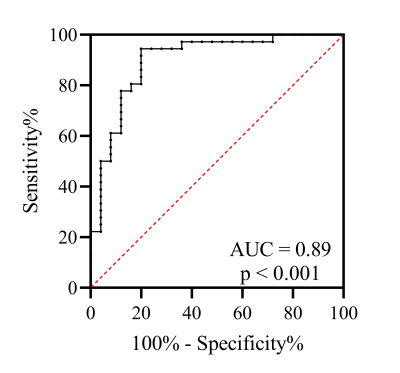
6. ECVMI was an independent predictor of final larger infarct size. The optimal cutoff value of ECVMI for the final larger infarct size predictor was 49.0% (Fig.4).
Discussion
T1 mapping can detect myocardial edema in acute MI4,5, and ECV provides the potential to quantitatively assess the severity of tissue disruption and loss of myocytes in the infarct region6. Our results suggested ECVMI was directly proportional to S2B time. In acute MI, with prolonged ischemia time, hypoxia of ischemic myocardium leads to anaerobic glycolysis and increased capillary permeability, degradation of cellar membrane and blood vessels in the ischemic zone leads to an increase in ECV7. The expected increase of native T1 in the infarct zone observed in the current study is attributed to an edematous reaction, which, however, did not show a correlation with total ischemia time as ECV did. The presence of MVO may affect the measurement of T1 values, as MVO reduced the MOLLI-measured native T1 in the infarct area8, and reduced blood supply in the MVO region also limiting myocardial edema. Native T1 value in the edema area was increased, while decreased in the MVO area, resulting in the uncertainty of native T1 value in the myocardial infarction area. ECV calculation is based on the T1 relaxation variation between pre-enhanced and post-enhanced T1-mapping images, the influence of paramagnetic effects between two images may be weakened, therefore, the interference of MVO on ECV is slight. Our study showed patients with higher ECVMI tended to have larger final infarct size during follow-up, which indicated ECVMI provides independent prognostic information beyond that provided by S2B time. What’s more, despite a strong correlation between total ischemic time and acute myocardial infarct size, the progressive change seems more pronounced in the longer ischemic time group. The possible reason may be that the infarct area contains both necrotic myocardium and structurally normal but functionally impaired myocardium, resulting in overestimating the necrotic tissue in the acute phase9.Conclusion
In STEMI, ECV of acutely infarcted myocardial may provide useful information for risk categorization, and clinically, we need to improve management systems to reduce total ischemic time.Acknowledgements
No acknowledgement found.References
1 B. Ibanez, S. James, S. Agewall, M.J. Antunes, C. Bucciarelli-Ducci, H. Bueno, et al., 2017 ESC Guidelines for the management of acute myocardial infarction in patients presenting with ST-segment elevation: The Task Force for the management of acute myocardial infarction in patients presenting with ST-segment elevation of the European Society of Cardiology (ESC), Eur Heart J, 39 (2018) 119-177. 2 A.J. Taylor, M. Salerno, R. Dharmakumar, M. Jerosch-Herold, T1 Mapping: Basic Techniques and Clinical Applications, JACC Cardiovasc Imaging, 9 (2016) 67-81.
3 S. Yu, J. Zhou, K. Yang, X. Chen, Y. Zheng, K. Zhao, et al., Correlation of Myocardial Strain and Late Gadolinium Enhancement by Cardiac Magnetic Resonance After a First Anterior ST-Segment Elevation Myocardial Infarction, Front Cardiovasc Med, 8 (2021) 705487.
4 H. Bulluck, S.K. White, S. Rosmini, A. Bhuva, T.A. Treibel, M. Fontana, et al., T1 mapping and T2 mapping at 3T for quantifying the area-at-risk in reperfused STEMI patients, J Cardiovasc Magn Reson, 17 (2015) 73.
5 E. Tahir, M. Sinn, S. Bohnen, M. Avanesov, D. Saring, C. Stehning, et al., Acute versus Chronic Myocardial Infarction: Diagnostic Accuracy of Quantitative Native T1 and T2 Mapping versus Assessment of Edema on Standard T2-weighted Cardiovascular MR Images for Differentiation, Radiology, 285 (2017) 83-91.
6 A. Kidambi, M. Motwani, A. Uddin, D.P. Ripley, A.K. McDiarmid, P.P. Swoboda, et al., Myocardial Extracellular Volume Estimation by CMR Predicts Functional Recovery Following Acute MI, JACC Cardiovasc Imaging, 10 (2017) 989-999.
7 R. Fernandez-Jimenez, J. Sanchez-Gonzalez, J. Aguero, J. Garcia-Prieto, G.J. Lopez-Martin, J.M. Garcia-Ruiz, et al., Myocardial edema after ischemia/reperfusion is not stable and follows a bimodal pattern: imaging and histological tissue characterization, J Am Coll Cardiol, 65 (2015) 315-323.
8 B.H. Chen, D.A. An, J. He, J.R. Xu, L.M. Wu, J. Pu, Myocardial extracellular volume fraction allows differentiation of reversible versus irreversible myocardial damage and prediction of adverse left ventricular remodeling of ST-elevation myocardial infarction, J Magn Reson Imaging, 52 (2020) 476-487.
9 N. Ojha, S. Roy, J. Radtke, O. Simonetti, S. Gnyawali, J.L. Zweier, et al., Characterization of the structural and functional changes in the myocardium following focal ischemia-reperfusion injury, Am J Physiol Heart Circ Physiol, 294 (2008) H2435-43.
Figures