4824
Improved strategy for diagnosing incidental benign and malignant lung nodules during cardiac MR using volumetric multi-contrast dark blood SSFP
Robert R Edelman1,2, Nondas R Leloudas1, Jianing Pang3, and Ioannis R Koktzoglou1,4
1Radiology, NorthShore University HealthSystem, Evanston, IL, United States, 2Radiology, Feinberg School of Medicine, Northwestern University, Chicago, IL, United States, 3Siemens Medical Solutions USA, Chicago, IL, United States, 4Pritzker School of Medicine, University of Chicago, Chicago, IL, United States
1Radiology, NorthShore University HealthSystem, Evanston, IL, United States, 2Radiology, Feinberg School of Medicine, Northwestern University, Chicago, IL, United States, 3Siemens Medical Solutions USA, Chicago, IL, United States, 4Pritzker School of Medicine, University of Chicago, Chicago, IL, United States
Synopsis
Keywords: Lung, Cancer, unbalanced steady state free precession
Cardiovascular MR is an invaluable diagnostic tool for the heart and great vessels. As with cardiac CT, it is imperative to carefully evaluate areas outside of the heart to exclude the presence of clinically relevant lesions such as pulmonary infiltrates or lung cancer. Unfortunately, existing CMR techniques are grossly inadequate for detecting and characterizing extra-cardiac lesions. We hypothesized that prototype volumetric dark blood SSFP techniques could overcome these limitations and tested them in patients undergoing CMR. In this pilot study, dark blood SSFP outperformed standard CMR techniques for the evaluation of incidental pulmonary lesions, including benign nodules and cancer.INTRODUCTION
Cardiovascular MR is an invaluable diagnostic tool for the heart and great vessels, with many thousands of exams performed annually throughout the world. As with cardiac CT, it is imperative to carefully evaluate areas outside of the heart to exclude the presence of clinically relevant extra-cardiac lesions such as enlarged mediastinal lymph nodes, pulmonary infiltrates, or lung cancer. Such incidental findings are not uncommon. For instance, potentially significant incidental findings were present in 23% of patients undergoing chest CT for suspected COVID-19 and 34% of patients undergoing CMR [1,2]. The need for accurate detection of malignant pulmonary nodules is clear since delayed diagnosis and treatment can have a dire impact on long-term survival. The detection of incidental benign lesions is also essential. For instance, in a patient with nonspecific delayed myocardial enhancement, the presence of mediastinal adenopathy and lung nodules can suggest cardiac sarcoidosis.Standard CMR protocols include balanced SSFP, dual inversion turbo spin-echo, T1/T2 mapping, and various delayed enhancement sequences [3]. Unfortunately, these techniques are grossly inadequate for evaluating the lungs and mediastinum and are far inferior to CT. Spatial coverage is limited, artifacts occur within the lungs and at lung-soft tissue interfaces, and suboptimal image contrast makes it difficult to identify extra-cardiac abnormalities. As a result, when patients undergo CMR, significant incidental lesions such as early-stage lung cancers are easily overlooked or misdiagnosed, and a major opportunity for early diagnosis and treatment is lost. There is therefore a critical unmet need to develop better techniques to detect and characterize incidental lesions during CMR, with the aim of eventually matching the excellent diagnostic performance of CT. To overcome the limitations of existing CMR techniques for evaluating extra-cardiac pathology, we propose the use of novel dark blood, susceptibility-insensitive 3D unbalanced steady-state free precession (SSFP) pulse sequences. We hypothesize that the dark blood contrast obtained with this new approach will prove advantageous for distinguishing clinically significant incidental lesions such as small, early-stage lung cancers from nearby blood vessels or cardiac structures. These techniques were evaluated in a pilot study of patients undergoing CMR examinations as well as in patients with lung nodules identified by CT.METHODS
The study was approved by the hospital institutional review board. Imaging was performed using 1.5 Tesla scanners (MAGNETOM Avanto Dot, Aera, or Sola, Siemens Healthcare, Erlangen, Germany).Standard pulse sequences for lung evaluation included 2D balanced steady-state free precession (bSSFP) HASTE, and volumetric interpolated breath-hold examination (VIBE). Two prototype versions of dark blood SSFP were studied: (1) 3D unbalanced SSFP (3D uSSFP) [4] and (2) 3D readout-balanced SSFP (3D RB-SSFP). These imaging techniques are respectively based on legacy fast imaging with steady-state precession (FISP) and reversed FISP (PSIF) pulse sequences. Typical scan parameters included: diastolic ECG gating, sampling bandwidth = 1184 Hz/pixel, gradient spoiler amplitude = 0.2 x imaging gradient amplitude, parallel acceleration (ipat) factor = 2, flip angle = 22 degrees. T1 and T2 weighting were obtained respectively by applying a saturation recovery magnetization preparation with a TI = 300 - 600 ms or an adiabatic T2 preparation with T2prep time = 60 – 120 ms. Lesion conspicuity and artifacts were evaluated by a single experienced observer using a 4-point scale, ranging from (1) non-diagnostic, lesion not assessable due to artifacts, to (4) excellent lesion conspicuity with negligible artifacts.RESULTS
Lesion conspicuity was best, and image artifacts least severe, with the prototype dark blood SSFP techniques (Figure 1). Compared with HASTE, lesion margins were substantially sharper and areas near the heart were better evaluated. Compared with VIBE, the dark blood contrast and suppression of ghost artifacts from the heart and blood vessels proved advantageous. Unlike bSSFP, dark blood SSFP provided sharp delineation of lesion margins without visible degradation by off-resonance effects. T2-weighted dark blood SSFP allowed the distinction of solid and cystic lesions, while T1-weighted dark blood SSFP enabled evaluation of lesion enhancement.DISCUSSION AND CONCLUSION
In this pilot study, volumetric multi-contrast dark blood SSFP outperformed standard CMR techniques for the evaluation of incidental pulmonary lesions, including benign nodules and cancer. The techniques are efficient, allowing the lungs to be evaluated in just a few breath-holds without the artifacts commonly seen using standard imaging techniques, while the use of magnetization-prepared versions allowed T1-weighted and T2-weighted dark blood images to be acquired for lesion characterization. Further study appears warranted to determine whether dark blood SSFP provides a clinically useful adjunct to standard CMR sequences for the detection and characterization of incidental extra-cardiac lesions.Acknowledgements
NIH grants 1R01CA263091 and 1R21CA273280.References
1) Kilsdonk ID, et al. Eur J Radiol Open. 2021;8:100366.
2) O'Sullivan JW, et al. BMJ. 2018;361:k2387.
3) Kramer CM, et al. J Cardiovasc Magn Reson. 2020;22(1):17.
4) Edelman RR, et al. J Cardiovasc Magn Reson. 2021;23(1):127.
Figures
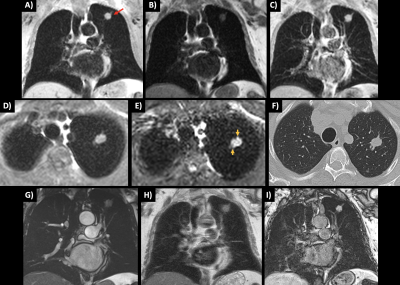
1. Small, early stage lung cancer found during CMR. A) 3D uSSFP shows the lesion (arrow). The lungs and blood vessels appear uniformly dark. B) Pre-Gd T1-weighted 3D uSSFP. C) Post-Gd T1-weighted 3D uSSFP shows lesion enhancement. D) Axial 3D uSSFP. E) T2-prepared 3D RB-SSFP shows lesion spiculations (short arrows). F) CT obtained one week following CMR shows similar findings. G) 2D bSSFP. H) HASTE shows blurring in the phase-encoding direction. I) VIBE depicts the lesion, but also shows artifacts in the lungs and inferior lesion-to-background contrast compared with dark blood SSFP.
DOI: https://doi.org/10.58530/2023/4824