4823
Intravoxel incoherent motion and diffusion kurtosis imaging can be used to assess the differentiation degree of non-small cell lung cancer1Lanzhou University Second Hospital, Lanzhou, China
Synopsis
Keywords: Lung, Lung, intravoxel incoherent motion, diffusion kurtosis imaging, differentiation degree, lung cancer
The purpose of this study was to assess differentiation degree of non-small cell lung cancer (NSCLC) by using intravoxel incoherent motion (IVIM) and diffusion kurtosis imaging (DKI) . There were statistically significant differences in D and Dapp values between the poorly differentiated group and the moderately and highly differentiated group (p>0.05). D value had the best diagnostic efficacy in evaluating the differentiation degree of NSCLC [area under the curve (AUC) =0.773]. Our study demonstrated that D value derived from IVIM and Dapp derived from DKI can distinguish the differentiation degree of NSCLC.Introduction
Lung cancer is the most frequently occurring malignant tumor in males and the leading cause of cancer death in men and women.1 And non-small cell lung cancer (NSCLC) accounts for approximately 85% of lung cancer cases.2 The differentiation degree of tumor is different, and the treatment method and prognosis are also different. Therefore, it is particularly important to accurately evaluate the differentiation degree of lung cancer. IVIM and DKI might provide more accurate information about water diffusion. IVIM is able to obtain diffusion (true diffusivity, D) and perfusion parameters (fraction of perfusion, f, and pseudo-diffusion parameter, D*) separately.3 DKI can reflect the diffusion of water molecules in non Gaussian distribution and the complexity of tissues.4 In this study, we assess the feasibility of IVIM and DKI to evaluate differentiation degree of NSCLC.Methods
Forty-one consecutive patients with NSCLC were enrolled in this study. MRI was performed within 1 week after finding lung lesions on CT. All Protocols were performed on a 3T MR scanner (GE Premier, GE Healthcare, Milwaukee, Wisconsin, USA). The lung images obtained included coronal T2WI, axial IVIM (repetition time/echo time, 7500/63ms; slice thickness, 4.0mm; interslice gap, 1mm; field of view, 512 ×512mm; and matrix, 256×256) and axial DKI (repetition time/echo time, 7200/70.8ms; slice thickness, 4.0mm; interslice gap, 1mm; field of view, 512 ×512mm; and matrix, 256×256). IVIM in three orthogonal directions was measured by using b values of 0, 20, 60, 100, 150, 200, 400, 600, 800, and 1000s/mm2. DKI in three orthogonal directions was measured by using b values of 0, 1000, and 2000s/mm2. Two radiologists independently analyzed the IVIM and DKI parameters for each lesion using post-processing software. The intraclass correlation coefficient (ICC) was generated to assess interobserver agreement. The parameters were compared between the poorly differentiated group and the moderately and highly differentiated group. Receiver operating characteristic analysis was performed to evaluate the diagnostic efficacy.Results
Intraobserver agreement was from good to excellent. Excellent interobserver agreement between the two observers was obtained for D, Dapp, Kapp and f with ICC of 0.931, 0.878, 0.840, and 0812 respectively. Good interobserver agreement was obtained for D* with ICC of 0.712. There were statistically significant differences in D and Dapp values between the poorly differentiated group and the moderately and highly differentiated group (p < 0.05), but D*, f, and Kapp showed no statistically significant differences between the two groups (Table 1). ROC curve analysis showed that the D value had the highest area under the curve (AUC = 0.773), followed by Dapp (AUC = 0.745)(Fig.1 and Table 2). Nevertheless, the difference in diagnostic efficacy among the two parameters was not statistically significant (p > 0.05). Representative case is shown in Fig.2 and 3.Discussion
In this study, we found that ADC and D values of moderately and highly differentiated group were significantly higher than those of poorly differentiated group, which is consistent with previous studies5, 6 Theoretically, as the differentiation degree of NSCLC decreases, the tissue atypia and the degree of malignancy increases, the proliferation of tumor cells will become more vigorous, leading to increased cell density and reduced extracellular space7. In this study, the perfusion-related parameters D* and f were not significantly different between the poorly differentiated group and the moderately and highly differentiated group. The reason may be that the repeatability of D* and f values in pulmonary diffusion imaging is poor and has great variability, which is affected by the shape, size and location of the lesion8. In this study, the ICC of D* was lower than other parameters.Conclusion
This study demonstrated that the diffusion parameter (D and Dapp) derived from IVIM and DKI could be used to noninvasively identify the differentiation degree of NSCLC.Acknowledgements
No.References
1 Sung H, Ferlay J, Siegel RL, et al. Global Cancer Statistics 2020: GLOBOCAN Estimates of Incidence and Mortality Worldwide for 36 Cancers in 185 Countries. CA Cancer J Clin2021;71:209-249.
2 Hsu WH, Yang JC, Mok TS, Loong HH. Overview of current systemic management of EGFR-mutant NSCLC. Ann Oncol2018;29:i3-i9.
3 Le Bihan D, Breton E, Lallemand D, Aubin ML, Vignaud J, Laval-Jeantet M. Separation of diffusion and perfusion in intravoxel incoherent motion MR imaging. Radiology1988;168:497-505.
4 Rosenkrantz AB, Padhani AR, Chenevert TL, et al. Body diffusion kurtosis imaging: Basic principles, applications, and considerations for clinical practice. J Magn Reson Imaging2015;42:1190-1202.
5 Zhou Y, Yang G, Gong XQ, et al. A study of the correlations between IVIM-DWI parameters and the histologic differentiation of hepatocellular carcinoma. Sci Rep2021;11:10392.
6 Li HW, Yan GW, Yang J, et al. Quantitative analysis for detection and grading of hepatocellular carcinoma: Comparison of diffusion kurtosis imaging, intravoxel incoherent motion and conventional diffusion-weighted imaging. Oncol Lett2022;24:403.
7 Kanauchi N, Oizumi H, Honma T, et al. Role of diffusion-weighted magnetic resonance imaging for predicting of tumor invasiveness for clinical stage IA non-small cell lung cancer. Eur J Cardiothorac Surg2009;35:706-710; discussion 710-701.
8 Jiang J, Yin J, Cui L, et al. Lung Cancer: Short-Term Reproducibility of Intravoxel Incoherent Motion Parameters and Apparent Diffusion Coefficient at 3T. J Magn Reson Imaging2018;47:1003-1012.
Figures
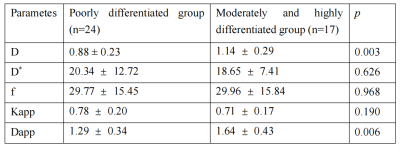
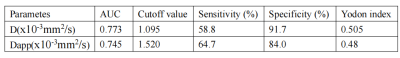
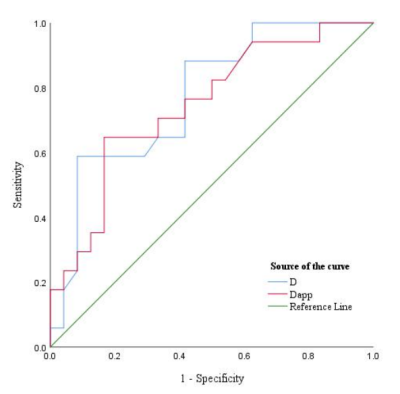
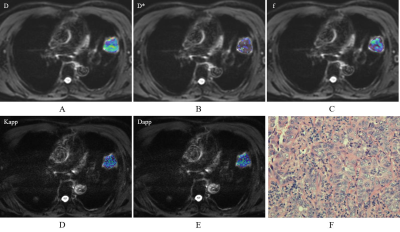
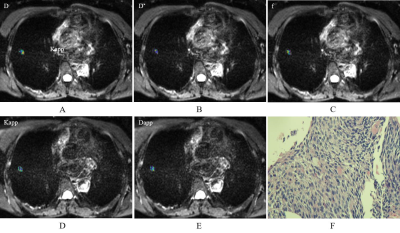
Fig.3 An 72-year-old male diagnosed with lung squamous cell carcinoma. (A) A diffusion map demonstrating a D value of 1.49×10-3 mm2/s. (B) A pseudodiffusion coefficient map demonstrating a D* value of 18.12×10-3 mm2/s. (C) A perfusion fraction map showing an f value of 17.92%. (D) A diffusion map showing a Dapp value of 1.83×10-3 mm2/s. (E) A kurtosis map showing a Kapp value of 0.43. (F) Hematoxylin and eosin (H&E) staining confirms the mass to be moderate-highly differentiated lung squamous cell carcinoma