4816
Remote Pneumatic Dose Administration for 129Xe MRI: Effects on Lung Inflation and Patient Experience
Alexander Church1, Shou Zhang1, Junlan Lu1, Cody Blanton1, Jennifer Korzekwinski1, David Mummy1, and Bastiaan Driehuys1
1Radiology, Duke University, Durham, NC, United States
1Radiology, Duke University, Durham, NC, United States
Synopsis
Keywords: Lung, Hyperpolarized MR (Gas), New Devices
Hyperpolarized 129Xe MRI requires repeatable lung inflation volumes to ensure consistent and accurate data. Current dose administration techniques require specialized study personnel to not only properly coach the subject through the inhalation maneuver, but also to directly administer the 129Xe dose, often while leaning deep into the MRI bore. Since lung inflation directly affects imaging data, it is important to maximize the consistency of inflation volumes across imaging sessions. We propose a novel 129Xe gas administration device intended to mitigate lung inflation differences as well as allow for remote administration of doses from outside the bore.
Purpose
Hyperpolarized 129Xe MRI produces high-resolution, non-invasive 3D imaging of pulmonary function. However, current dose administration approaches typically require dedicated personnel to coach subjects through a breathing maneuver and deliver the dose. This process entails coaching subjects to inhale/exhale several times and then positioning the mouthpiece, manually releasing the contents of the dose bag, and prompting the subject to breathe in rapidly1. This is further challenged by the confined space and limited visibility in the scanner bore, since the dose mouthpiece must be inserted into the subject's mouth at precisely the time of end exhalation. Although seasoned personnel can perform this technique adeptly, it is inefficient and can lead to imperfect inhalations, delays, and confusion, especially when subjects inadvertently breathe in room air or begin inhaling the dose at the wrong point of the breathing cycle. This last point is particularly crucial as the key to making 129Xe images highly repeatable is to ensure that subjects start inhalation from a well-defined lung volume2,3. Here, we demonstrate and test a pneumatic device that allows subjects to take their preparatory breaths with the mouthpiece and dose already in place, with study personnel actuating release of the dose remotely. We provide an initial comparison of this method vs conventional manual delivery by comparing the repeatability of lung inflation levels in the resulting images, as well as surveying subjects regarding their experience.Methods
The pneumatic device (Figure 1) was designed to be injection molded from medical grade polymers and takes the place of the typical mouthpiece on the dose bag assembly. The interior pneumatic piston (thermoplastic elastomer) has built in seals and includes a center through-bore that allows the passage of room air prior to actuation. It is housed within a high-density polyethylene body and retainment cap, onto which a mouthpiece is fitted. All injection molded parts (Protolabs) were assembled in-house and involved light greasing of the piston, installing in the body, and gluing on the retainment cap. Actuation is achieved via positive pressure provided by a 10 ml syringe attached to a length of capillary tubing (Figure 2). The device is reusable for each subject and can be reset to the room air setting by applying negative pressure via the same syringe.To evaluate device impact on lung inflation repeatability and patient experience, healthy subjects were recruited (n=9) to undergo breath hold proton MRI and respond to survey questionnaires (Figure 3). Images were acquired using a breath-hold 3D radial acquisition according to the 129Xe consortium protocol1. Room air dose volumes were tailored based on ~20% of forced vital capacity (FVC), which was rounded to either 500, 750, or 1000 ml. Subjects were randomized to first inhale air by either conventional (manual) dose delivery or by using the remote administration device, after which imaging was repeated with the other method. After a 15 minute break, they then underwent a second imaging session in which the two delivery approaches were repeated in reverse order. After the first scan of each administration method, subjects responded to a brief questionnaire assessing their anxiety level, comfort, and overall experience. During the second of these surveys, they were asked which method (if any) they preferred.
Each of the four proton scans (2 for each administration method) were segmented using an automated deep learning-based algorithm that generated a mask to define the thoracic cavity volume4. The resulting volumes were compared to measure inflation repeatability achieved with the two delivery methods. Questionnaire results were analyzed using Fisher’s exact test to determine preference for either delivery method.
Results
All subjects completed all four scans without incident. Lung inflation (Figure 4A+4B) was repeatable to within 0.45±0.37L with remote administration as compared to 0.51±0.50L with manual delivery. A p-value of 0.5 indicated no significant difference between the delivery methods overall. The minimum inflation difference detected using either delivery method was 0.05L.A preliminary analysis of questionnaire results is shown in Figure 5. None of the responses were significantly different for either anxiety, comfort, or overall quality of the experience. However, there was a trend towards subjects having an overall preference for manual delivery while preferring the relative comfort of the remote delivery method.
Discussion
This study illustrates that remote, pneumatic delivery of 129Xe is feasible and well-tolerated. This method can reduce the complexity of the delivery procedure by enabling the dose to be placed in the subject’s mouth and remain there during preparatory breaths, after which the MRI technologist can remotely release the gas contents and start the scan.Preliminary analysis of imaging lung volumes suggests that remote delivery device provided a ~12% decrease in lung inflation difference between repeat sessions. Given the well-known inflation dependence of 129Xe gas exchange metrics such as Membrane:Gas and RBC:Gas, this improvement is encouraging2,3. (We also note that deep learning-based thoracic segmentations were not manually corrected, which may have led to minor imperfections in segmentation).
Survey results indicate that the new method is at least equally well-tolerated as conventional delivery approaches. Future studies conducted with a larger sample size will permit a comprehensive assessment of the quantitative and patient-experience characteristics of this new dose delivery system relative to conventional dose delivery methods.
Acknowledgements
NSF GRFP DGE-1644868, R01HL105643, R01HL12677References
- Niedbalski PJ, Hall CS, Castro M, Eddy RL, Rayment JH, Svenningsen S, Parraga G, Zanette B, Santyr GE, Thomen RP, Stewart NJ, Collier GJ, Chan HF, Wild JM, Fain SB, Miller GW, Mata JF, Mugler JP 3rd, Driehuys B, Willmering MM, Cleveland ZI, Woods JC. Protocols for multi-site trials using hyperpolarized 129 Xe MRI for imaging of ventilation, alveolar-airspace size, and gas exchange: A position paper from the 129 Xe MRI clinical trials consortium. Magn Reson Med. 2021 Dec;86(6):2966-2986. doi: 10.1002/mrm.28985. Epub 2021 Sep 3. PMID: 34478584.
- Hahn AD, Kammerman J, Evans M, Zha W, Cadman RV, Meyer K, Sandbo N, Fain SB. Repeatability of regional pulmonary functional metrics of Hyperpolarized 129 Xe dissolved-phase MRI. J Magn Reson Imaging. 2019 Oct;50(4):1182-1190. doi: 10.1002/jmri.26745. Epub 2019 Apr 10. PMID: 30968993; PMCID: PMC6750965.
- Hughes PJC, Smith L, Chan HF, Tahir BA, Norquay G, Collier GJ, Biancardi A, Marshall H, Wild JM. Assessment of the influence of lung inflation state on the quantitative parameters derived from hyperpolarized gas lung ventilation MRI in healthy volunteers. J Appl Physiol (1985). 2019 Jan 1;126(1):183-192. doi: 10.1152/japplphysiol.00464.2018. Epub 2018 Nov 9. PMID: 30412033; PMCID: PMC6383640.
- Leewiwatwong S, Lu J, Mummy D, et al Deep learning-based thoracic cavity segmentation for hyperpolarized 129Xe MRI. International Society for Magnetic Resonance in Medicine Annual Meeting 2021 p0391
Figures
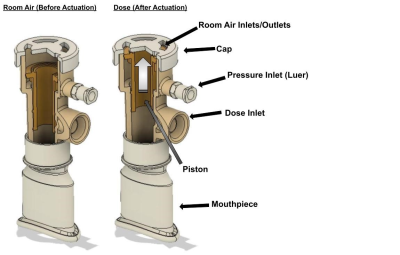
Figure 1. A cutaway view of the remote dose administration device before and after actuation. The center bore of the orange piston acts as the flow path for room air during preparatory breaths, and the large 90-degree fitting acts as the flow path from the dose post actuation. Multiple seals are used to accomplish two functions from the actuation, both to release the dose as well as seal the device from room air. The device itself is separate from the mouthpiece, allowing for removal or adjustment.
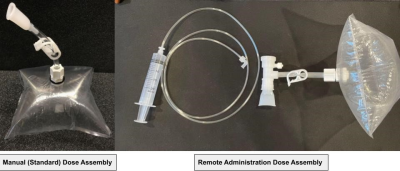
Figure 2. Demonstrative examples of the manual delivery and remote delivery dose assemblies. As mentioned, the remote delivery device takes the place of the manual delivery’s mouthpiece on the length of the dose bag tubing. 1/16 inch capillary tubing is attached to a 10 ml syringe and then to the pressure port of the device.

Figure 3. The device permits the dose to be placed in the subject’s mouth prior to scanning. The technologist can coach the subject and remotely actuate release of the dose as they initiate the scan. A length of capillary tubing connected to a 10 ml syringe acts as the pressure source for actuation and reset of the pneumatic piston within the device. The removable mouthpiece allows for the dose bag to be placed either to the side of the subject’s head. The subject can breathe normally and take their preparatory air breaths with the device in place.

Figure 4. Box plots demonstrating the overall lung inflation values and lung inflation difference for both dose administration methods across the two BHUTE imaging sessions. The spread of the remote delivery device is slightly larger in both 4A and 4B compared to the manual delivery, but symmetrical concerning inflation differences in 4B. The manual delivery box (4B) indicates a bias towards lower inflation difference between the two scanning sessions. A single subject accounted for the maximum outliers for both dose delivery methods.
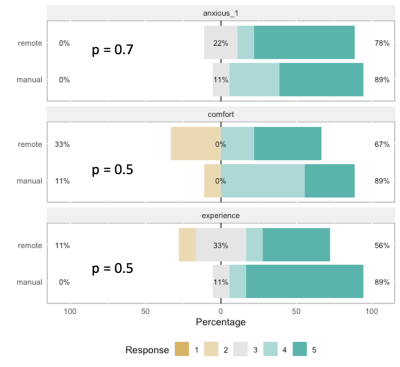
Figure 5. Stacked bar charts showing the response to the first session questionnaire concerning subject anxiety, comfort, and overall experience compared for the two dose delivery methods. P-values for each set of results were calculated using Fisher’s exact test. No significant difference between the two administration types was found.
DOI: https://doi.org/10.58530/2023/4816