4813
3D Free-Breathing Ultrashort Echo Time (UTE) 1H Ventilation Compared with Hyperpolarized 129Xe Ventilation
Fei Tan1, Rachel L. Eddy2,3, Vanessa M. Diamond2, Jonathan H. Rayment2,4, and Peder E. Z. Larson1,5
1UC Berkeley-UCSF Graduate Program in Bioengineering, University of California, Berkeley and University of California, San Francisco, San Francisco, CA, United States, 2BC Children's Hospital Research Institute, Vancouver, BC, Canada, 3Centre for Heart Lung Innovation, University of British Columbia, Vancouver, BC, Canada, 4Department of Pediatrics, University of British Columbia, Vancouver, BC, Canada, 5Department of Radiology and Biomedical Imaging, University of California, San Francisco, San Francisco, CA, United States
1UC Berkeley-UCSF Graduate Program in Bioengineering, University of California, Berkeley and University of California, San Francisco, San Francisco, CA, United States, 2BC Children's Hospital Research Institute, Vancouver, BC, Canada, 3Centre for Heart Lung Innovation, University of British Columbia, Vancouver, BC, Canada, 4Department of Pediatrics, University of British Columbia, Vancouver, BC, Canada, 5Department of Radiology and Biomedical Imaging, University of California, San Francisco, San Francisco, CA, United States
Synopsis
Keywords: Lung, Lung
This abstract compares the 3D UTE 1H ventilation calculated from Motion-Compensated Low-Rank constrained reconstruction (MoCoLoR) with the hyperpolarized 129Xe ventilation for validation. The dataset covers healthy volunteers and pediatric and adult patients with cystic fibrosis (CF). We validated that 3D UTE 1H has a positively correlated VDP with the gold standard 129Xe and a high spatial VDP accuracy.Introduction
Imaging-based quantification of ventilation can provide critical information for the characterization of lung disease. Noble gas MRI, such as hyperpolarized (HP) 129Xe MRI, can directly image the airspaces in the lung (1). It has high contrast and serves as a gold standard for ventilation imaging. Whereas 129Xe MRI requires specialized MRI equipment and is limited to few specialized research centers worldwide, 1H UTE-based ventilation can be acquired on any MR scanner and therefore more readily available.Ultrashort-echo time (UTE) 1H lung MRI is applicable for ventilation map calculation. Motion-resolved reconstruction (2,3) techniques provide image volumes at multiple respiratory states. Ventilation can be calculated indirectly through the regional volume difference between the states. This abstract compares the 3D UTE 1H ventilation calculated from motion-compensated low-rank constrained reconstruction (MoCoLoR) (4,5) with the HP 129Xe ventilation for validation.
Methods
AcquisitionThe study was approved by the University of British Columbia Research Ethics Board (REB). Twenty-four subjects (ages 29.1±14.7 y/o, 14M) including healthy volunteers, pediatric and adult patients with cystic fibrosis (CF) were included.
Each subject inhaled HP 129Xe/nitrogen gas mixture and went through a 2D multi-slice 129Xe spoiled gradient recalled (GRE) sequence during breath-holding. Total inhaled gas and 129Xe doses were based on height (6). Volume-matched 1H images were acquired using the body coil with room air inhaled. The two sequences were acquired with the same FOV=40cmx30-40cm, slice thickness=15mm, and #slices=12-17.
A variable density 3D radial UTE sequence (7) was adopted for the UTE 1H acquisition during free-breathing. The key parameters were: FOV=35cm isotropic, resolution=1.37mm isotropic, #spokes=100,000, TE/TR=0.07/2.88ms. All images were acquired on a 3T clinical scanner (Discovery MR750, GE Healthcare).
129Xe Ventilation
Xenon images for each subject were processed using the linear-binning method (8) for ventilation defect quantification. The thoracic cavity was segmented from the 2D multi-slice 1H images using a region-growing approach. Afterward, the Xe volume was normalized by its 99th percentile, and values less than 0.16 within the thoracic cavity were defined as ventilation defects. This threshold was determined by two standard deviations below the mean ventilation from a healthy volunteer cohort. Ventilation defect percent was calculated as the ventilation defect volume normalized to the volume-matched 1H thoracic cavity volume.
UTE 1H Ventilation
Phase-resolved UTE 1H image volumes were reconstructed using the Motion-Compensated Low-Rank (MoCoLoR) approach. Briefly, this method jointly reconstructs respiratory motion states with a low-rank penalty and uses iteratively refined deformable image registration between states to reduce the rank. Since it uses all data jointly in the reconstruction, it is very SNR efficient, similar to the iMoCo method (9). The regional ventilation was calculated by the Jacobian determinant of the motion field at the end-inspiration state over the end-expiration state minus one. Lastly, regional ventilation underwent the same linear binning approach for ventilation defect quantification to minimize bias from VDP processing algorithms.
Figure 1 summarizes the processing pipeline.
Results
Figure 2 illustrates a representative case with a high Xe VDP of 43.48%. The ventilation defect segmentations from Xe and UTE 1H (Figure 2c) have significant overlap areas. UTE 1H correctly predicted the ventilation defects on the left and right middle and superior regions.Figure 3 shows ventilation results from a patient with a mild ventilation defect. As shown in Figure 3c, the UTE 1H ventilation defect overlaps with the 129Xe ventilation defect at the posterior of the lung. The anterior ventilated region is also correctly classified.
Figure 4 plots the relationships of the VDP between 129Xe and UTE 1H across all subjects. According to the correlation plot, VDP from both methods ranges from 0 to 0.5, and the ventilation defect percentages from Xenon and proton positively correlate. The Bland-Altman plot suggests a bias of 0.00 and limits of agreement of 0.20.
Figure 5 demonstrates the spatial accuracy of the ventilation defect segmentation. Accuracy is defined as (overlapped ventilation defect region + overlapped ventilated region)/total lung volume. This metric mitigates dice coefficient's strong dependency on the actual VDP value. The accuracy of UTE 1H was between 0.49 to 0.70. Note that this accuracy value is susceptible to small differences in image registration, which is challenging given there was typically some motion between Xe and UTE scans.
Discussion
UTE 1H ventilation is positively correlated with the gold standard 129Xe ventilation with moderate-to-high accuracy for VDP quantification between the two methods. We note that these two methods quantify ventilation in different respiratory maneuvers. UTE 1H is acquired dynamically during 5-min tidal breathing. In contrast, Xe is acquired during a static ~10s breath-hold of a fixed volume from functional residual capacity. In addition, since the UTE 1H ventilation is an indirect measurement, a lower value could also reflect changes in increased stiffness/decreased compliance of that region of the lung. These factors may contribute to the difference in ventilation defect regions.Conclusion
In conclusion, we validated 3D UTE 1H ventilation against 129Xe ventilation. It demonstrates a positively correlated VDP with the gold standard 129Xe and a high spatial VDP accuracy. UTE 1H MRI ventilation may be implemented on any MR scanner and has the potential to be widely implemented to provide clinically-relevant ventilation information for patients with lung disease.Acknowledgements
No acknowledgement found.References
1. Mugler JP, Altes TA. Hyperpolarized 129 Xe MRI of the human lung. J. Magn. Reson. Imaging 2013;37:313–331 doi: 10.1002/jmri.23844.2. Jiang W, Ong F, Johnson KM, et al. Motion robust high resolution 3D free-breathing pulmonary MRI using dynamic 3D image self-navigator: Motion Robust High-Resolution 3D Pulmonary MRI. Magn. Reson. Med 2018;79:2954–2967 doi: 10.1002/mrm.26958.
3. Feng L, Axel L, Chandarana H, Block KT, Sodickson DK, Otazo R. XD‐GRASP: Golden‐angle radial MRI with reconstruction of extra motion‐state dimensions using compressed sensing. Magn. Reson. Med. 2016;75:775–788 doi: 10.1002/mrm.25665.
4. Tan F, Zhu X, Larson P. Motion-Compensated Low-Rank Reconstruction with Iterative Registration for Ventilation Analysis on Ultrashort Echo Time (UTE) Lung MRI. In: ; 2022.
5. Zhu X, Ong F, Lustig M, Larson P. Motion Compensated Low-Rank(MoCoLoR) constrained reconstruction with application to motion resolved lung MRI. In: ; 2020.
6. Smith LJ, Horsley A, Bray J, et al. The assessment of short- and long-term changes in lung function in cystic fibrosis using 129 Xe MRI. Eur Respir J 2020;56:2000441 doi: 10.1183/13993003.00441-2020.
7. Johnson KM, Fain SB, Schiebler ML, Nagle S. Optimized 3D ultrashort echo time pulmonary MRI. Magnetic Resonance in Medicine 2013;70:1241–1250 doi: 10.1002/mrm.24570.
8. He M, Driehuys B, Que LG, Huang Y-CT. Using Hyperpolarized 129Xe MRI to Quantify the Pulmonary Ventilation Distribution. Academic Radiology 2016;23:1521–1531 doi: 10.1016/j.acra.2016.07.014.
9. Zhu X, Chan M, Lustig M, Johnson KM, Larson PEZ. Iterative motion‐compensation reconstruction ultra‐short TE (iMoCo UTE) for high‐resolution free‐breathing pulmonary MRI. Magn Reson Med 2020;83:1208–1221 doi: 10.1002/mrm.27998.
Figures
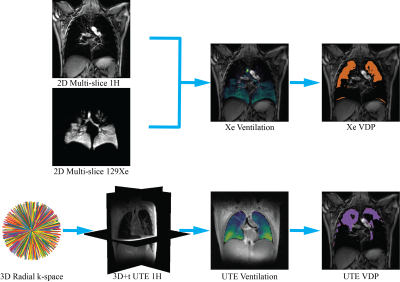
Figure 1. Processing pipeline for 129Xe ventilation and UTE 1H ventilation. 2D multi-slice 1H and 129Xe were used for the 129Xe ventilation map and ventilation defect percentage calculation. 3D radial UTE 1H k-space data were reconstructed using motion-compensated low-rank reconstruction. Motion fields from registration were used for UTE ventilation calculation. Lastly, the UTE 1H volume was registered to the 2D multi-slice 1H image using non-rigid registration, and the transforms were applied to the UTE 1H ventilation map for direct comparison.
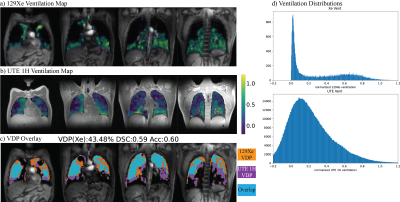
Figure 2. Representative results for a subject with high ventilation defect 43.48%. a) Xe ventilation overlaid on the 2D multi-slice 1H image, where the transparency represents ventilation. b) normalized UTE 1H ventilation overlaid on UTE 1H images, lower values correspond to poor ventilation. c) VDP overlay of 129Xe and UTE 1H. d) ventilation distributions show that both normalized 129Xe and UTE 1H ventilation have positive skew, suggesting poor ventilation in most of the lungs.
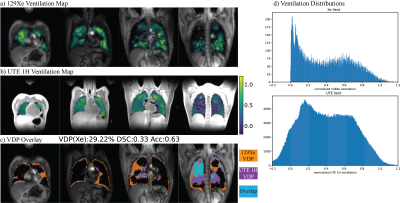
Figure 3. Representative results for a subject with mild ventilation defect 29.22%. The ventilation defect regions at the posterior of the lung from 129Xe and UTE 1H overlap.
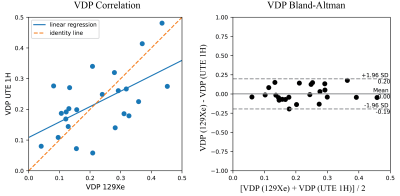
Figure 4. Correlation and Bland-Altman plots between 129Xe Ventilation Defect Percentage (VDP) and UTE 1H VDP for all patients.
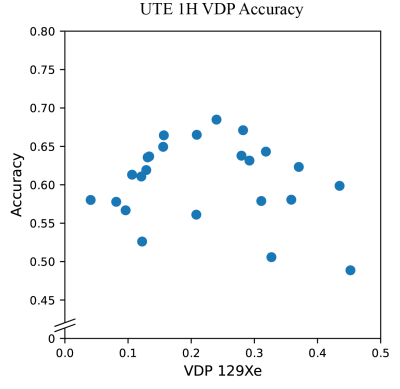
Figure 5. The spatial accuracy of UTE 1H VDP after registering to 129Xe for all patients. Accuracy is defined as (overlapped ventilation defect region + overlapped ventilated region) / total lung volume. Note that these absolute accuracy results are sensitive to the accuracy of registration between the UTE and 129Xe data, which was in some cases challenging due to motion between scans and the different contrast between the 2D GRE used for 129Xe localization and 3D UTE.
DOI: https://doi.org/10.58530/2023/4813