4790
Clinical Viability of AI-enabled 0.5T MRI Scanner to Improve Access
Arjun Narula1, Uday Patil2, Anand SH3, Harikrishnan Raveendran4, Shailaja Muniraj5, Pallavi Rao6, Anurita Menon6, Allison Nicole Garza7, Santosh Kumar7, Gautam Kumar7, Srinivas NR7, Syam Babu7, Ravi Jaiswal7, Rajagopalan Sundaresan7, Ashok Kumar Reddy7, Sajith Rajamani7, Rajdeep Das7, Nitin Jain7, Sudhir Ramanna7, Sundar V7, Florintina Charlaas7, Sudhanya Chatterjee7, Rohan Patil7, Megha Goel7, Dattesh Shanbhag7, Vikas Kumar Anand7, Abhishek Galagali7, Sathish KV7, Preetham Shankpal7, Harsh Kumar Agarwal7, Suresh Emmanuel Joel7, and Ramesh Venkatesan7
1Narula Diagnostics, Rohtak, India, 2Manipal Hospitals, Bangalore, India, 3Jivaa Diagnostics, Tumkur, India, 4Core Clinico PET Imaging, Thane, India, 5Prima Diagnostics, Bangalore, India, 6Image Core Lab, Bangalore, India, 7GE Healthcare, Bangalore, India
1Narula Diagnostics, Rohtak, India, 2Manipal Hospitals, Bangalore, India, 3Jivaa Diagnostics, Tumkur, India, 4Core Clinico PET Imaging, Thane, India, 5Prima Diagnostics, Bangalore, India, 6Image Core Lab, Bangalore, India, 7GE Healthcare, Bangalore, India
Synopsis
Keywords: Machine Learning/Artificial Intelligence, Low-Field MRI, Accessible MRI
We validate the clinical viability of a 0.5T scanner to reduce cost and improve access to quality MRI using AI based IQ enhancement to compensate for IQ reduction due to lower field and other lower hardware specifications. We obtained data from 65 patients from the re-ramped 0.5T and a commercially available 1.5T MRI system for brain and cervical spine. Radiologists compared image quality between the two and rated the image on the ability to perform diagnosis. We observed that more than 90% of the images were rated to be above diagnostic levels and AI reconstruction significantly improved the image quality.Introduction
MRI is the imaging modality of choice for full body imaging, especially soft tissue imaging due to its excellent soft tissue contrast and absence of ionizing radiation. However, due to cost and expertise needed to use the scanner and interpret the images, access to use of MRI is limited to higher income patient population and geographical regions. Access to MRI will improve population clinical outcomes. MRI could be made accessible by reducing the cost (both capital cost and total cost of ownership) by using a lower field strength scanner along with lower gradient and RF specifications (Geethanath, S. et al., 2019). Conventional imaging with these lower hardware specifications will degrade image quality and clinical usability. Poor image quality may lead to missed abnormalities and reduced confidence in reporting. Leveraging the recent developments in artificial intelligence (AI)-based image acquisition and reconstruction, images from these accessible systems could be enhanced to improve radiologist confidence in reporting. In addition to improving access, lower field also provides additional advantages over higher field strength scanners; for example, in lung imaging and imaging with implants and imaging in presence of implants (Marques JP et al., 2019; Hori M et al., 2021; Lavrova, et al., 2022). Here we present results on images from patients using a 0.5T scanner in a semi-urban hospital in India with AI-enabled reconstruction and compared the image quality with a commercial 1.5T MR system.Methods and Materials
A GE Creator (GE Healthcare, Milwaukee) 1.5T scanner was modified to operate at 0.5T with modified transmit and receive chain electronics. Custom made 12-channel HNU coil was used to image the brain and cervical spine. 65 Patients were scanned at a diagnostic center with conventional clinical scan on the commercial 1.5T scanner along with 3 to 6 clinically relevant series on the 0.5T scanner after informed consent and fulfilling inclusion and exclusion criteria in an institutional IRB approved study. The series obtained for brain and cervical spine are shown in Table 1. Scan duration, coverage and resolution were maintained comparable between the 0.5T and the 1.5T scanners (Table 1). The raw data obtained from the 0.5T scanner was reconstructed using custom built AI-reconstruction, a modified AirTM Recon DL (GE Healthcare; Lebel RM, 2020) method. AI-reconstructed images along with the corresponding commercial 1.5T scanner images were shown to up to 3 radiologists (randomly selected out of the pool of 5 radiologist, each having minimum of 10 years of experience with MR images) to compare image quality. We also obtained image quality ratings on a subset of conventional non-AI reconstructed images from the 0.5T scans from 1 radiologist and performed a paired comparison between AI-reconstructed images and non-AI-reconstructed images. Image quality (IQ) was obtained from radiologists using a Likert scale between 1 and 9 (Table 2), where any IQ score 5 and above is diagnostically acceptable.Results
A total of 210 series (excluding localizers) were obtained from 65 patients. Typical images are shown in Figure 1. AI reconstructed DICOM series were rated for image quality by 2-3 radiologists. Out of the 210 series, 190 series were above diagnostic level (Likert score > 5) and only 20 series were rated below diagnostic level. Likert rating over 210 series had an average of 6.27 ± 1.19. The average distribution of ratings of radiologists are shown in figure 2 and per contrast is shown in Table 3. There was very low inter-rater variability among radiologists on image quality rating: inter-rator ratings difference was 1.73 ± 1.12. Of the 20 series rated below diagnostic image quality, 5 were due to excessive motion artifacts, 2 were due to RF interference noise, 7 were poor quality brain SWAN images, 6 were poor quality c-spine images due to CSF pulsation artefacts.Wilcoxon paired signed rank test between AI reconstructed images and non-AI reconstructed images showed statistically significant IQ improvement (5.3 ± 1.38 vs. 7.3 ± 1.65, p<5e-14).Discussion & Conclusions
AI image reconstruction improved the image quality of 0.5T MRI system to above diagnostic image quality when compared with 1.5T commercial MR system. 90% of image series have diagnostic image quality or better rating and of the remaining 10%, few sequences (brain-SWAN and Spine-T2) had scope for improvement. Minor protocol modifications like addition of flow compensation or changing PE direction, will improve the IQ of these sequences also. The remainder of the unacceptable images were rated poorly because of motion and interference artifacts. AI based reconstruction had a significant improvement in the image quality of the images. In the C-Spine subset of data that were compared between AI-reconstrcted and conventional reconstructed, when AI-based reconstruction was not used, the images were on the boundary of diagnostic value (Likert score of ~5) and with the help of AI, almost all images were at or above diagnostic image quality. Low inter-rater variability also showed these results are consistent among radiologists.These results point in the direction that AI-reconstructed images from 0.5T MRI produced clinically acceptable images for brain and spine and could be used in improve IQ of potentially more affordable scanners improving access. Conclusions on clinical feasibility of accessible scanners on other anatomies and contrasts needs further investigation.Acknowledgements
No acknowledgement found.References
Geethanath S, Vaughan JT. Accessible magnetic resonance imaging: A review. J Magn Reson Imaging, Vol 49:7 pp e65–77, 2019.
Hori M et al., Low-Field Magnetic Resonance Imaging: Its History and Renaissance. Invest Radiol. Vol 56:11 pp 669–79, 2021.
Lavrova A et al., “Initial Evaluation of Neuroimaging at 0.55T”, Proceedings of the ISMRM 2022.
Lebel RM, “Performance characterization of a novel deep learning-based MRimage reconstruction pipeline”, https://arxiv.org/pdf/2008.06559.pdf, 2020.
Marques JP et al., “Low-field MRI: An MR physics perspective”, JMRI Vol 49:6 pp 1528-1542, 2019.
Figures
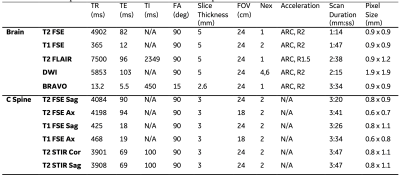
Table 1: Protocol specifications used for brain and C-Spine
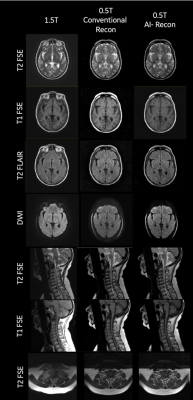
Figure 1: Typical images from the 0.5T scanner for head and C-Spine and the corresponding 1.5T Creator image from the same patient.
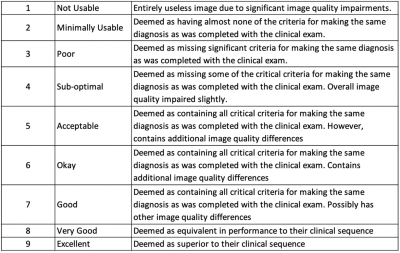
Table 2: Likert scale rating for image quality
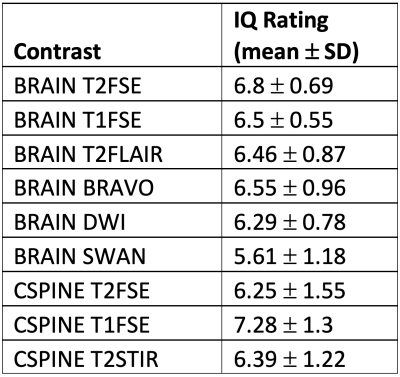
Table 3: Mean Radiologist IQ rating scores of each contrast
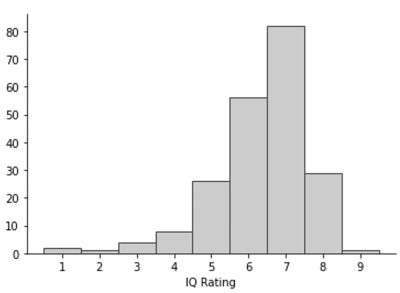
Figure 2: Distribution of image quality rating by radiologists on a likert scale of 1-9 (where 5 and above do not lose any diagnostic information).
DOI: https://doi.org/10.58530/2023/4790