4789
Investigation of DWI with Deep Learning-based Reconstruction in the Differentiation of Benign and Malignant Breast Lesions1Department of Radiology, Sun Yat-Sen University Cancer Center, Guangzhou, China, 2MR Research, GE Healthcare, Beijing, China
Synopsis
Keywords: Machine Learning/Artificial Intelligence, Diffusion/other diffusion imaging techniques
As the most common malignant tumor in women, the differentiation of benign lesion from malignant breast tumors is the most essential step in early diagnosis. Recent study demonstrated that DWI could offer great help in differential diagnosis of breast tumors. The novel deep learning-based reconstruction (DLR) technique is able to increase SNR of MRI images. Using DLR, DWI images can be acquired with less NEX (fast DWI) and still maintain the image quality. This study indicated the feasibility of fast DWI protocol with DLR in the differentiation of breast benign lesions and malignant tumors.Introduction
Early diagnosis and tumor differentiation of breast cancer are crucial to form a systematic treatment with better survival rate for such a common malignant tumor in women1, 2. Diffusion weighted imaging (DWI) with apparent diffusion coefficient (ADC) could provide characterization of water molecule diffusivities in breast benign and malignant lesions, which gives oncologists a better and clearer version for an accurate diagnosis3. Due to its low signal-to-noise ratio (SNR), the EPI-based DWI methods were often acquired with multiple number-of-excitations (NEX). However, multi-NEX protocol might lead to a long and unpleasant scan time. Recently, the deep learning-based reconstruction (DLR) technique has been proven to increase SNR of MRI images. Previous studies indicated the potential of DLR in offering better image quality of MRI images within a single scan4, 5. In this study, we performed DWI protocols with varied NEX and DLR conditions to investigate their image qualities and the capability in the differentiation of breast benign and malignant lesions.Methods
In total, fifteen patients with twelve benign and eleven malignant lesions were include in this study. It was approved by IRB and written informed consent was obtained for every subject. All patients were scanned on a GE SIGNA Premier 3T MRI scanner. For each patient, three different DWI protocols were conducted. Two b-values, 50 and 800 s/mm2, were acquired with the following NEX and DLR conditions. G1: conventional DWI protocol, NEX = 2, 8 for each b-value and no DLR. G2: fast DWI protocol, NEX = 1, 4 for each b-value, no DLR. G3: fast DWI protocol, NEX = 1, 4 for each b-value, with DLR technique for image reconstruction. All protocols were acquired with other parameters as follows: TR = 2500 ms; TE = minimum; slice sickness = 5 mm with 1 mm spacing; FOV = 34 cm × 34 cm; image matrix = 128 × 128 ; a total scan time of G1 was 2 min 30 sec, G2 was 1 min 30 sec and G3 was 1 min 30 sec.The ADC, SNR and contrast-to-noise ratio (CNR) values of region-of-interests (ROIs) were calculated for the evaluation of image quality and diagnostic performance. All ROIs were manually placed on lesions based on contrast-enhanced images by an experienced radiologist. The receiver operating characteristic (ROC) curve was plotted and the area under ROC curve (AUC) was calculated to assess the performance of each DWI protocol in differentiating benign and malignant breast lesions. Statistical analyses of differences among three DWI protocols for all patients were performed using repeated measure ANOVA tests with Bonferroni correction. For all tests, p < 0.01 was considered statistically significant.Results
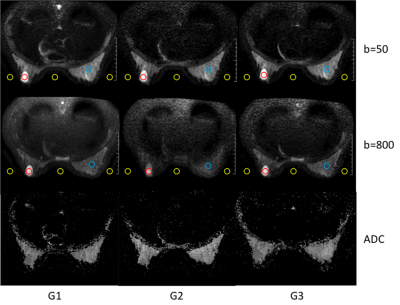
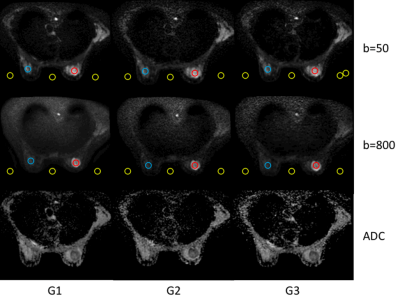
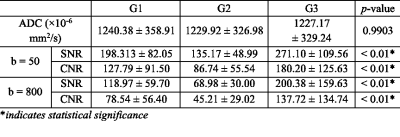
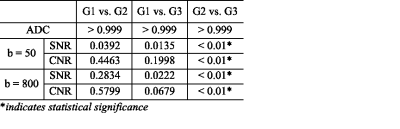
Imaging results of different DWI protocols from a representative patient with benign and malignant were depicted in Figure 1 and 2, respectively. Higher SNR and better image quality of DWI images from fast DWI with DLR in both figures were shown compared with the ones from fast DWI protocol without DLR. Compared with benign lesions (red ROIs), the malignant lesion shows restricted diffusivity as reported3. Table 1 showed the numerically values of ADC, SNR and CNR of various DWI protocols, where significant differences at SNR and CNR values were detected but no difference for ADC results. Pairwise comparisons of each two protocols were demonstrate in Table 2. As it was shown in this table, DLR technique can significantly improve SNR of DWI images for fast DWI protocol (G2 vs G3). Moreover, fast DWI protocol with DLR had similar SNR, CNR and ADC values compared with conventional DWI protocol. The ROC curves of three DWI protocols for the differentiation of benign and malignant breast lesions were illustrated in Figure 3. The AUC values of three protocols were 0.8333 (G1, 95% CI: 0.622–1.045), 0.8333 (G2, 95% CI: 0.622–1.045), and 0.8864 (G3, 95% CI: 0.721–1.052). It indicated the best performance of fast DWI protocol with DLR.Discussion and conclusion
In this study, DLR technique was shown to significantly increase the image quality of fast DWI protocols for patients with breast lesions. In addition, fast DWI protocol with DLR technique could achieve similar image qualities and comparative ADC values compared with conventional multi-NEX DWI protocol. At last, the fast DWI protocol with DLR had the best performance in the differentiation of breast benign and malignant lesions. Therefore, the feasibility of clinical applications of DLR based fast imaging DWI protocol was proved in this study.Acknowledgements
No acknowledgement found.References
1. Siegel, Rebecca L., Kimberly D. Miller, and Ahmedin Jemal. "Cancer statistics, 2019." CA: a cancer journal for clinicians 69.1 (2019): 7-34.
2. Byers, Tim, et al. "The American Cancer Society challenge goal to reduce US cancer mortality by 50% between 1990 and 2015: results and reflections." CA: a cancer journal for clinicians 66.5 (2016): 359-369.
3. Zhang, Michelle, et al. "Multiparametric MRI model with dynamic contrast‐enhanced and diffusion‐weighted imaging enables breast cancer diagnosis with high accuracy." Journal of Magnetic Resonance Imaging 49.3 (2019): 864-874.
4. Hahn, Seok, et al. "Image quality and diagnostic performance of accelerated shoulder MRI with deep learning–based reconstruction." American Journal of Roentgenology 218.3 (2022): 506-516.
5. Sreekumari, A., et al. "A deep learning–based approach to reduce rescan and recall rates in clinical MRI examinations." American Journal of Neuroradiology 40.2 (2019): 217-223.
Figures