4761
Alternations of Brain Local Cortical Thickness in Adult Schizophrenia: A Surface-Based Morphometry Meta-Analysis1Medical Imaging Center, First Affiliated Hospital of Jinan University, Guangzhou, China, 2Department of Radiology, Six Afliated Hospital of Sun Yat-sen University, Guangzhou, China, 3MR Research, GE Healthcare, Beijing, China
Synopsis
Keywords: Psychiatric Disorders, Brain, Schizophrenia; Cortical thickness; Surface-based morphometry; Meta-Analysis
Numerous neuroimaging studies have revealed abnormalities in specific brain regions in schizophrenia (SCZ), but results have been inconsistent. We conducted a whole-brain meta-analysis on surface-based morphometry studies between patients with SCZ and healthy controls by using the Seed-based d Mapping with Permutation of Subject Images (SDM-PSI) software. The meta-analysis demonstrated that SCZ exhibits abnormalities in cortical thickness in the inferior frontal gyrus, insula, and superior temporal gyrus. The results expand the current understanding of cortical thickness abnormalities in patients with SCZ, which would provide promising targets for therapeutic intervention.Introduction
Schizophrenia (SCZ) is a severe psychiatric disease characterized by cognitive impairment, auditory hallucination, delusions, abnormal behavioral disorders, and poor long-term prognosis leading to adverse effects on the life quality and social function of patients with SCZ1-4. SCZ affects approximately 1% of the general population in the world, places a tremendous burden on sufferers, families, and society, and remains a debilitatingly progressive and incurable disease5. It is recognized globally as the most significant reason for a chronic psychiatric disability. However, the specific pathophysiology and neuroanatomical biomarkers of SCZ remain elusive. Structural magnetic resonance imaging is a non-invasive neuroimaging technique widely used to research brain structural abnormalities in SCZ, significantly improving our understanding of the neurobiological characteristics of Schizophrenia6,7. Cortical thickness is one of the critical indicators of brain structure, mainly measured by surface-based morphometry (SBM), reflecting the size, density, and arrangement of neurons, neuroglia, and nerve fibers8 and changes with typical development, aging, and specific pathologies9. Thus, there is an increasing number of exploratory studies on cortical thickness in SCZ patients. Although significant progress has been made in understanding the neurobiological characteristics of SCZ, previous studies have reported inconsistent alterations in cortical thickness in SCZ patients. These inconsistencies may be due to differences between studies in the sample characteristics (such as age, sexuality, and ethnicity), illness duration, flexible analyses and statistical methods and stage. Thus, a quantitative assessment of cortical thickness abnormalities using neuroimaging meta-analysis is needed to overcome such divergence in the SCZ literature.Methods
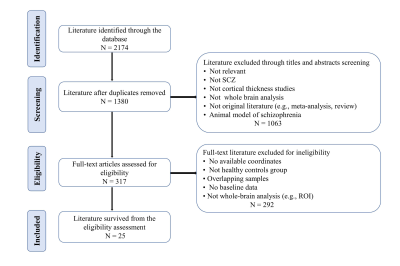
This meta-analysis of the whole-brain study explored cortical thickness alteration in SCZ patients across ethnicity, first-episode patients with SCZ, and chronic patients with SCZ compared with healthy controls (HCs) by using the Seed-based d Mapping with Permutation of Subject Images (SDM-PSI) software. A total of 25 studies (33 datasets) comprising 2008 SCZ patients and 2004 HCs were included in a systematic literature search. Of the patients with SCZ, 23.01% were first-episode patients (7 studies), 44.02% were chronic patients (14 studies), and 32.97% did not report accurate illness duration of patients. Furthermore, 45.62% of patients (11 studies with 14 experiments) were from Eastern countries (China and Japan), and 54.38% of patients (14 studies with 19 experiments) were from Western countries (America, Europe, Australia, Brazil, and Canada).Results
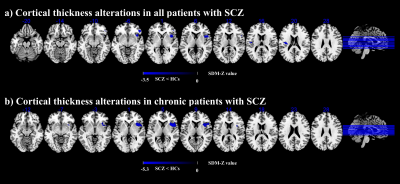
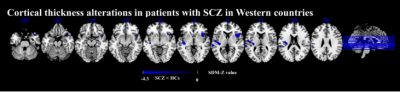
Overall, the principal results demonstrated that adult patients with SCZ displayed a decrease in cortical thickness in the right inferior frontal gyrus (IFG) and bilateral insula. Subgroup exploratory meta-analysis reported that individuals with chronic SCZ patients showed decreased cortical thickness in the right insula extending to the right IFG and right insula. Individuals with Western countries’ SCZ showed decreased cortical thickness in the right insula extending to the right IFG, left insula, and left superior temporal gyrus (STG). However, Patients with SCZ from Eastern countries showed no significant alterations in cortical thickness.Conclusions
The SBM meta-analysis suggested that SCZ patients showed aberrant cortical thickness mainly in the IFG, insula, and STG, suggesting that deficits in those regions might underlie the SCZ. In addition, inconsistent alteration in SCZ patients across ethnicity may draw attention to the disparity in multi-cultural consideration in SCZ research and help to demonstrate the pathophysiology of SCZ.Acknowledgements
The study was supported by grants from the National Natural Science Foundation of China (81671670, 81971597 and 82102003); National Key Research and Development Program of China (2020YFC2005700); Project in Basic Research and Applied Basic Research in General Colleges and Universities of Guangdong, China (2018KZDXM009); Key-Area Research and Development Program of Guangdong Province (2020B1111100001); Medical Science and Technology Research Foundation of Guangdong Province (A2021109). The funding organizations played no further role in study design, data collection, analysis and interpretation and paper writing.References
1. SHI D, LI Y, ZHANG H, et al. Machine Learning of Schizophrenia Detection with Structural and Functional Neuroimaging [J]. Dis Markers, 2021, 2021: 9963824.
2. PENADES R, SEGURA B, INGUANZO A, et al. Cognitive remediation and brain connectivity: A resting-state fMRI study in patients with schizophrenia [J]. Psychiatry research Neuroimaging, 2020, 303: 111140.
3. CARMONA I C, KUMBHARE D, BARON M S, et al. Quintuple AISI 1010 carbon steel core coil for highly focused transcranial magnetic stimulation in small animals [J]. AIP ADVANCES, 2021, 11(2).
4. BLAY M, ADAM O, BATION R, et al. Improvement of Insight with Non-Invasive Brain Stimulation in Patients with Schizophrenia: A Systematic Review [J]. J Clin Med, 2021, 11(1).
5. BAE Y, KUMARASAMY K, ALI I M, et al. Differences Between Schizophrenic and Normal Subjects Using Network Properties from fMRI [J]. J Digit Imaging, 2018, 31(2): 252-61.
6. PALANIYAPPAN L, MAAYAN N, BERGMAN H, et al. Voxel-Based Morphometry for Separation of Schizophrenia From Other Types of Psychosis in First-Episode Psychosis: Diagnostic Test Review [J]. Schizophr Bull, 2016, 42(2): 277-8.
7. CHIN R, YOU A X, MENG F, et al. Recognition of Schizophrenia with Regularized Support Vector Machine and Sequential Region of Interest Selection using Structural Magnetic Resonance Imaging [J]. Sci Rep, 2018, 8(1): 13858.
8. NARR K L, TOGA A W, SZESZKO P, et al. Cortical thinning in cingulate and occipital cortices in first episode schizophrenia [J]. Biol Psychiatry, 2005, 58(1): 32-40.
9. LI L, ZHANG Y, ZHAO Y, et al. Cortical thickness abnormalities in patients with post-traumatic stress disorder: A vertex-based meta-analysis [J]. Neurosci Biobehav Rev, 2022, 134: 104519
Figures