4734
Deep learning-based high-resolution T2-weighted imaging elevated clarity of prostatic calcification and diagnostic efficacy1Radiology, Renmin Hospital of Wuhan University, Wuhan, China, 2GE Healthcare, MR Research China, Beijing, China
Synopsis
Keywords: Prostate, Prostate
Prostatic calcification is common in benign prostatic hyperplasia (BPH) and usually asymptomatic. Our study showed the prostate T2WIDL images have higher subjective rating scores, clearer lesion contrast and improved detection rate of prostatic calcification, higher SNR and CNR. In addition, T2WIDL more clearly and sharply displayed prostate capsule, lesion contrast, prostate calcification and anatomical details Therefore, AIR™ Recon DL based T2WI (T2WIDL) quality in prostate MRI offer higher overall image quality and elevated a younger radiologist’s diagnostic performance on prostate calcification.Purpose
Deep learning (DL) technology has been widely applied in prostate MRI image segmentation, tumor detection, diagnostic efficacy and lesion local invasiveness with improved image resolution without losing image quality and adding scanning time 1-4. Prostatic calcification is common in benign prostatic hyperplasia (BPH) and affects the severity of symptoms of lower urinary tract symptoms (LUTS) 5. Prostatic calcification is usually asymptomatic and its presence is easily ignored in conventional T2WI (T2WIC) 6. Our study aimed to exam diagnosis efficacy on prostatic calcification and evaluate image quality of deep learning (AIR™ Recon DL) based T2WI (T2WIDL) by radiologists with fewer than 1 years of experience in prostate MRI compared to the other with 7 years of experience using T2WIC as reference.Methods
Seventy-eight patients (mean age : 67.1 ± 9.9) who underwent prostate MRI examinations (T2WIC and T2WIDL with the same parameters: TR=3483ms, TE=102ms. NEX= 2, FOV=180 × 180 mm2, matrix=288 × 256, and scan time 2 min 51 s ) were included in this retrospective study. Double-blinded evaluation was performed by both one- and seven-year experienced radiologists. The subjective evaluation contains image quality of A: prostate capsule; B: lesion contrast and edge sharpness; C: anatomical details (urethra、zone of prostate、seminal vesicle); D: skeleton and muscle clarity; E: overall image quality using the Likert Scale (5 = excellent, 1 = very poor) and prostatic calcification (0 = none, 1 =unsure, 2= existence), and then the intra‑/inter‑observer agreement were tested using κ statistics. The objective evaluation included the signal-to-noise ratio (SNR) and contrast-to-noise ratio (CNR), and paired t test or Mann-Whitney U test were used for statistical analysis according to data normality and equality of variance .Results
In terms of the subjective scores, overall image quality scores were rated significantly superior by both readers on T2WIDL compared to on T2WIC (reader 1: 4.6 ± 0.6 and 4.3 ± 0.7; reader 2: 3.4 ± 0.7 and 3.0 ± 0.8; P < 0.05, Figure 1) and inter-reader agreement was moderate (κ=0.7 , p<0.05) . For T2WIDL, the score consistency ranged from 0.6 to 0.8; there were significant differences in the scores between the two readers only for A: anatomical details and E: overall image quality(P<0.05). In terms of objective evaluation, T2WIDL showed significantly higher SNR and CNR than T2WIC (P < 0.05). The SNR of T2WIC and T2WIDL in benign and malignant lesions were 12.4 ± 2.4, 28.7 ± 8.1 and 10.1 ± 1.8, 27.7 ± 5.4, respectively, with significant differences (P < 0.01). There was no significant difference in CNR between benign and malignant lesions with and without DL (P > 0.05).Discussion and conclusions
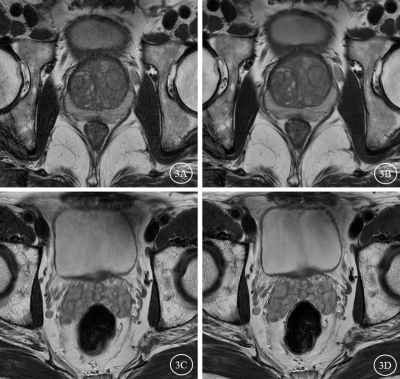
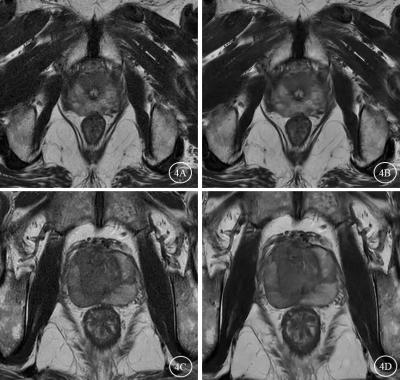
MRI is the optimal imaging examination method for the diagnosis of prostate diseases 7, and the image quality is always concerned. Patients with prostate calcification cannot be ignored especially in patients with BPH and prostatitis. For the relationships of periurethral calcification (PUC) severity and location with LUTS 8-9. In this work, we applied a novel DL-based MRI reconstruction method (T2WIDL) to investigate its impact on image quality compared to conventional T2WIC image. Our study showed the prostate T2WIDL images have high subjective rating scores, clearer lesion contrast and prostatic calcifications, high SNR and CNR. T2WIDL images are clearer and sharper in the display of prostate capsule, lesion contrast, prostate calcification and anatomical details (Figure 2-4), which is helpful for lesion identification and diagnosis, and the accurate identification of the presence of prostate calcification is helpful for early clinical intervention and delaying the worsen subjective LUTS symptoms 6. Therefore, the novel DL denoising reconstruction technique is helpful to improve the image quality of prostate T2WI.Acknowledgements
We thank Guangnan Quan and his team from the GE Healthcare, MR Research China, Beijing, for providing the scan guide, and especially thank to our team members Xinyang Song and Yufan Gao for their early work.References
[1]. Turkbey B. Better Image Quality for Diffusion-weighted MRI of the Prostate Using Deep Learning [J]. Radiology, 2022, 303(2): 382-383.
[2]. Takagi H, Kadoya N, Kajikawa T, et al. Multi-atlas-based auto-segmentation for prostatic urethra using novel prediction of deformable image registration accuracy [J]. Med Phys, 2020, 47(7):3023-3031.
[3]. Jans LBO, Chen M, Elewaut D, et al. MRI-based Synthetic CT in the Detection of Structural Lesions in Patients with Suspected Sacroiliitis: Comparison with MRI [J]. Radiology, 2021, 298(2): 343-349.
[4]. Kim M, Kim HS, Kim HJ, et al. Thin-Slice Pituitary MRI with Deep Learning-based Reconstruction: Diagnostic Performance in a Postoperative Setting [J]. Radiology, 2021, 298(1): 114-122.
[5]. Han JH, Kwon JK, Lee JY, et al. Is periurethral calcification associated with urinary flow rate and symptom severity in men with lower urinary tract symptoms-benign prostatic hyperplasia? Aretrospective review. Urology, 2015, 85(5): 1156-1161.
[6]. Yu SH, Lim DG, Kim SO. Clinical significance of distally located periurethral calcification in patients with lower urinary tract symptoms of benign prostate hyperplasia. Asian J Androl. 2022 Aug 2. Epub ahead of print. PMID: 35946225.
[7]. Turkbey B, Brown AM, Sankineni S, et al. Multiparametric prostate magnetic resonance imaging in the evaluation of prostate cancer [J]. CA Cancer J Clin, 2016, 66(4):326-336.
[8]. Han JH, Kwon JK, Lee JY, et al. Is periurethral calcification associated with urinary flow rate and symptom severity in men with lower urinary tract symptoms-benign prostatic hyperplasia? A retrospective review. Urology, 2015, 85(5): 1156–1161.
[9]. Han JH, Lee JY, Kwon JK, et al. Clinical significance of periurethral calcification according to the location in men with lower urinary tract symptoms and a small prostate volume. Int Neurourol J, 2017, 21(3):220-228.
Figures
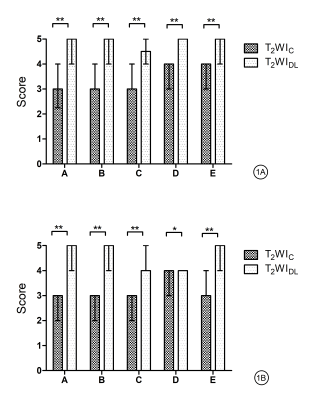
Comparison of qualitative image analysis between reader 1 and 2 for T2WI with and without DL. All data were expressed in terms of median (upper and lower quartiles). A: Reader 1 with one years of experience ; B: Reader 2 with seven years of experience. The asterisks represent a statistically significant difference (P < 0.05); *,P < 0.05;**,P < 0.01. The evaluation indicators of T2WI including: A-prostate capsule; B- lesion contrast and edge sharpness; C-anatomical details (urethra、zone of prostate、seminal vesicle); D-skeleton and muscle clarity; E-overall image quality.
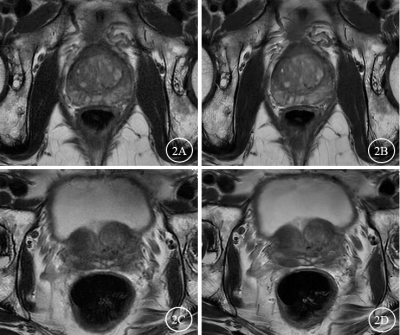
Images from a 71‑year‑old man diagnosed with BPH with a PSA level of 2.63 ng/ml. A,C: T2WIC, B,D: T2WIDL. The T2WIDL image showed a clearer contrast of the BPH lesion and pseudocapsule, while T2WIDL image also had better illustration for seminal vesicle.
Images A and B from a 75‑year‑old man diagnosed with PCa (GS=5+3=8), with a PSA level of 19.9 ng/ml; Images C and D from an 85‑year‑old man diagnosed with PCa (GS=5+4=9), with a PSA level of 88.3 ng/ml. A, C: T2WIC, B, D: T2WIDL. The T2WIDL image showed a clearer contrast and edge sharpness of the prostate cancer (PCa) lesion.