4733
Quantitative Analysis and Scan Time Impact of DL Recon Applied to Single-Shot Diffusion of the Prostate1GE Healthcare, Boston, MA, United States, 2Massachusetts General Hospital, Boston, MA, United States
Synopsis
Keywords: Prostate, Diffusion/other diffusion imaging techniques
Increasing the speed of multiparametric prostate MRI (mpMRI) is highly desirable. However, usual tradeoffs between signal-to-noise (SNR) and scan time must be considered and impact on quantitative metrics must be analyzed. One recently proposed approach applied a commercialized deep learning reconstruction (DL Recon) to prostate T2-weighted imaging, leveraging the capabilities of the DL algorithm to achieve a robust, high-quality T2-weighted acquisition in half the time. As such, this work focuses on evaluating the DL Recon on diffusion weighted imaging, which shows promise to cut acquisition time by ~70% and therefore benefit mpMRI.Introduction
Multiparametric Prostate MRI (mpMRI) protocols consist of high resolution multiplanar T2, diffusion weighted imaging (DWI), and dynamic contrast enhanced (DCE) acquisitions1. An ideal mpMRI protocol meeting or exceeding PIRADS® v2.12 recommendations can take ~25 minutes, even after optimizing protocols using commercially available acceleration techniques based on conventional multichannel parallel imaging. The biggest time sinks within these protocols are the T2 weighted and high b-value DWI acquisitions. There have been several recent publications focusing on shortening the scan time for these two acquisitions without loss in diagnostic quality3-5. One study focused on utilizing a novel, commercialized deep learning reconstruction (DL Recon) technology (AIR™ Recon DL, GE Healthcare)6 to reduce the multiplanar T2 acquisition time by 3-fold, without loss in signal-to-noise ratio (SNR)3. The purpose of this study is the application of this DL reconstruction technology to single-shot DWI acquisitions in the prostate. We focus on comparisons of the DL reconstruction to conventional reconstructions without loss in quantitative analysis, as well as the benefits in scan time reduction.Methods
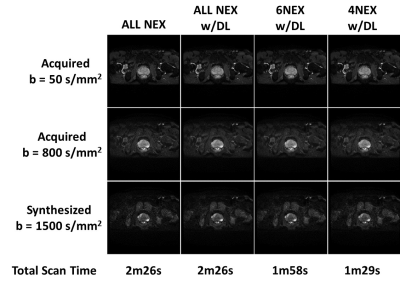
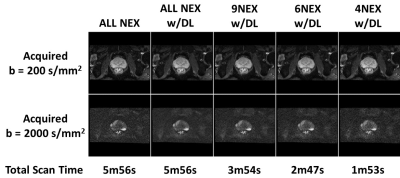
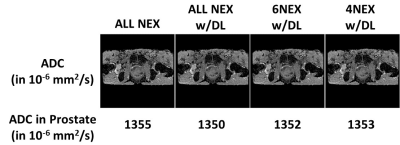
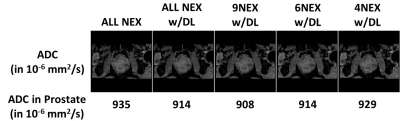
25 patients were scanned using the standard mpMRI clinical protocol at MGH, on a GE Signa Premier 3T MRI system (GE Healthcare, Waukesha, WI, USA). The protocol consists of axial, sagittal, and coronal T2 weighted scans, Large FOV and FOCUS DWI scans, and a DCE scan. The parameters for the Large FOV DWI scans are as follows: Matrix size=128x128; FOV=32x32cm2; Slice thickness=3mm; TR/TE=4705/53.4ms; b-values = 50/800 s/mm2; number of averages = 2/8; synthetic 1500 s/mm2; Total Scan Time=2min26s. The parameters for the FOCUS DWI scans are as follows: Matrix size=132x80; FOV=20x12cm2; Slice thickness=4mm; TR/TE=4500/59.2ms; b-values = 200/2000 s/mm2; number of averages = 8/18; Total Scan Time=5min56s. The DWI raw data were reconstructed in two ways, first using the product 2D cartesian reconstruction and second using the commercialized DL Recon algorithm, which is based on a Convolutional Neural Network (CNN) trained to remove ringing, reduce noise, and increase sharpness6. To assess the impact of reducing the number of averages (NEX) and by extension scan time, we applied the DL Recon to the raw data with a manual reduction in NEX (from 8 to 4 or 6 for Large FOV DWI/from 18 to 4, 6, or 9 for FOCUS DWI). The reconstructions were labeled as follows: ALL NEX, ALL NEX w/DL, and #NEX w/DL, where ALL indicates all averages were kept in reconstruction, and # indicates 4, 6, or 9 averages were kept in reconstruction. Within the DL Recon, images were reconstructed with a tunable noise reduction factor set to 50%. ADC maps were calculated in READY View (GE Healthcare, Waukesha, WI, USA) for all reconstructed scans, both across the whole volume and within the prostate in a representative slice. SNR was calculated in a representative slice of the prostate for the highest acquired b-values for both Large FOV DWI (b = 800 s/mm2) and FOCUS DWI (b = 2000 s/mm2). The standard deviation of the signal of an ROI in the obturator internus muscle served as the noise. An independent t-test was used for statistical analysis, with the ALL NEX conventional reconstruction serving as the gold standard, and p<0.05 deemed statistically significant.Results
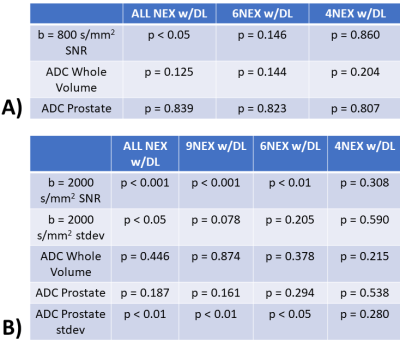
Figures 1 and 2 show representative Large FOV and FOCUS DWI images, respectively, across all b-values and all reconstructions, along with the resulting scan time. Figures 3 and 4 show representative ADC maps calculated from the dataset shown in Figures 1 and 2, respectively. Qualitatively, the images with DL Recon applied showed less noise and increased sharpness as more NEX were kept in the reconstruction. Even at only 4NEX in both Large FOV and FOCUS DWI cases, the images looked comparable to the conventional reconstruction with ALL NEX. Figure 5 summarizes the statistical analysis for each DWI acquisition based on the NEX chosen. Even with only 4NEX, compared to the conventional reconstruction with ALL NEX, there was no statistical difference in SNR or ADC for either Large FOV or FOCUS DWI acquisitions. However, the scan time was calculated to be reduced by up to ~40 and ~70% compared to the conventional acquisitions for Large FOV and FOCUS DWI, respectively.Discussion
In this study, the proposed abbreviated DWI scans offer a clinically viable method to reduce scan time by up to 70% while retaining sufficient SNR thanks to DL Recon. Furthermore, this reduction in scan time does not incur any penalty in quantitative analysis, as evidenced by no statistical difference in ADC values. These encouraging results warrant a continuation of the study, including increasing the cohort size and calculating CNR in abnormal cases to better understand the effect of DL Recon on identifying prostatic malignancies. In conclusion, DL Recon offers a new strategy to reduce scan time in mpMRI of the prostate by alleviating the need to collect multiple averages for DWI acquisitions.Acknowledgements
No acknowledgement found.References
1. O’Shea et al. “PI‑RADS: multiparametric MRI in prostate cancer,” Magnetic Resonance Materials in Physics, Biology and Medicine 2022, Vol. 35, 523-532.
2. Turkbey et al. “Prostate imaging reporting and data system version 2.1: 2019 update of prostate imaging reporting and data system version 2,” European Urology 2019, Vol.76, 340–51.
3. O’Shea et al. “Initial experience in abbreviated T2-weighted Prostate MRI using a Deep Learning reconstruction,” ISMRM 2020 #2450.
4. Ueda et al. “Deep Learning Reconstruction of Diffusion-weighted MRI Improves Image Quality for Prostatic Imaging,” Radiology 2022, Vol. 303, 373-381.
5. Kaye et al. “Accelerating Prostate Diffusion-weighted MRI Using a Guided Denoising Convolutional Neural Network: Retrospective Feasibility Study,” Radiology: Artificial Intelligence 2020, Vol. 2, e200007.
6. Lebel, RM. “Performance characterization of a novel deep learning-based MR image reconstruction pipeline,” arXiv 2020.
Figures