4712
Subendocardial Involvement as an Underrecognized LGE Subtype Related to Adverse Outcomes in Hypertrophic Cardiomyopathy1Fuwai Hospital, Beijing, China
Synopsis
Keywords: Cardiomyopathy, Heart
In a retrospective cohort study, 497 consecutive HCM patients with LGE confirmed by cardiac MR were collected. The risk of cardiovascular events increases with per percentage increase in LGE extent in HCM patients with extensive LGE (>15%). While instead of LGE extent, the subendocardium-involved LGE pattern, an underrecognized phenotype in HCM, is related to the adverse outcomes in patients with non-extensive LGE (<15%), especially for heart failure-related outcomes. RVIP LGE is commonly seen in HCM, but this LGE location does not merit a prognostic value.PURPOSE
Late gadolinium enhancement (LGE) has been established as an independent predictor for adverse outcomes in hypertrophic cardiomyopathy (HCM)1. With mounting evidence that the presence and the extent of LGE provide important prognostic values in HCM, extensive LGE (≥15% of LV mass) has been assembled into the risk-stratification algorithm for HCM]2. A recent study revealed that the increase in LGE extent seemed barely influence the risk of adverse events in HCM patients with non-extensive LGE (<15% of LV mass)3, so we hypothesized that specific LGE subtypes might correlate to clinical outcomes in these patients. Several studies showed a rare LGE pattern with subendocardial involvement without ischemic etiology4-5. Besides, LGE involving the location of right ventricle insertion point (RVIP) is most commonly seen in HCM, which is related to high mechanical stress6. However, the prevalence and clinical significance of these LGE subtypes have not been well demonstrated. Thus, we aim to investigate the prognostic value of subendocardium-involved LGE pattern and RVIP LGE location in HCM patients.METHODS
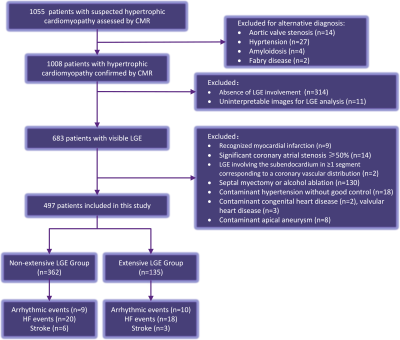
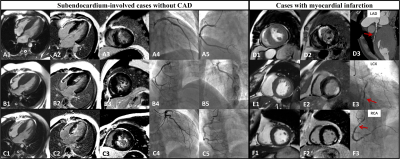
In this single-center retrospective study, we evaluated 1055 patients diagnosed as HCM by cardiac MR between June 2012 and June 2014. After exclusion, a total of 497 HCM patients were included (Figure 1). Representative cases without CAD showing subendocardium-involved LGE pattern (A-C) and representative cases with CAD showing myocardial infarction (D-F) are displayed in Figure 2. Endpoints included a composite of heart failure events, arrhythmic events, and stroke. Unlike well-defined stripe-like LGE located in coronary artery territories in myocardial infarction, subendocardium-involved LGE in HCM patients majorly exhibited patchy hyperenhancement that distributed dispersively in subendocardium or amorphous hyperenhancement occupied subendocardial area with vague margin. A cubic spline model was used to study the shape of the relationship between LGE extent and clinical outcome. Univariate and multivariate Cox proportional hazard regression analyses were performed to identify independent predictors of the endpoint events.RESULTS
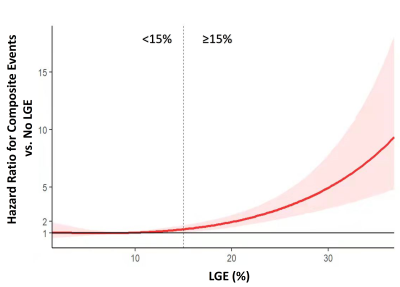
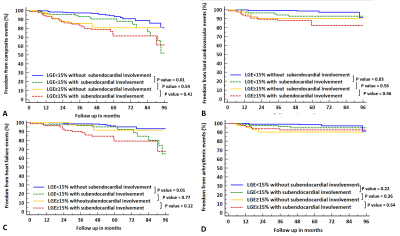
According to the LGE extent with a cutoff of 15%, the cohort was then divided into two groups: extensive LGE group (n=135, age: 45.4 ± 12.2 years; 87 males) and non-extensive LGE group (n=362, age: 45.9±13.5 years; 252 males). Subendocardium-involved LGE was observed in 37.0% (184/497) patients with positive LGE and 18.3% (184/1008) of the total HCM population; the number for RVIP LGE was 83.3% (414/497) and 41.1% (414/1008), respectively. Compared to patients with non-extensive LGE, extensive LGE group had more patients with subendocardial involvement (68.9% vs. 25.1%, P<0.001) and RVIP LGE (95.6% vs. 78.7%, P<0.001). Over the follow-up duration for a median of 57.9 months in HCM patients with LGE, a total of 66 patients (13.3%) experienced composite events. 35 composite events occurred in non-extensive group; 31 composite events occurred in extensive LGE group. Patients with extensive LGE had a significantly higher annual incidence of adverse events (5.1%/year vs. 1.9%/year, P<0.0001). Spline analysis showed a non-linear association between LGE extent with hazard ratios for composite endpoints (Figure 3): the incidence of composite endpoint was not closely related to LGE extent in non-extensive LGE group, while the risk of composite endpoint increased with per percentage increase in LGE amount in extensive LGE group. LVEF<50% (HR, 9.82; 95% CI: 5.60-17.24, p<0.001), atrial fibrillation (HR, 3.69; 95% CI: 2.23-6.11, p<0.001), and nonsustained ventricular tachycardia (HR, 2.14; 95% CI: 1.23-3.73, p=0.007) were selected as adjustment variables by univariate Cox regression analysis for composite endpoints in all patients. In univariate analysis, instead of LGE extent and the presence of RVIP LGE, subendocardium-involved LGE pattern was related to composite events, hard cardiovascular events, and HF events in non-extensive LGE group. After adjusting for LVEF<50%, atrial fibrillation, and nonsustained ventricular tachycardia, subendocardium-involved LGE was still identified as an independent predictor for composite events (HR, 2.12; 95% CI: 1.06-4.24, p=0.03). In extensive LGE group, instead of the presence of RVIP LGE and subendocardium-involved LGE, LGE extent was related to composite events, hard cardiovascular events, and HF events in univariate analysis; After adjustment, the extent of LGE significantly correlated to composite endpoints (HR, 1.05; 95% CI: 1.00-1.10, p=0.03). The multivariate-adjusted analyses for hard cardiovascular events, HF events, and arrhythmic events were not performed due to the limited number of events. Furthermore, Kaplan-Meier analysis showed a significantly increased risk of composite events (Figure 4A; log-rank p=0.01), hard cardiovascular events(Figure 4B; log-rank p=0.03), and HF events (Figure 4C; log-rank p=0.01) in non-extensive LGE group with subendocardial involvement, but no risk of arrhythmic events increased (Figure 4D).CONCLUSIONS
The risk of cardiovascular events increases with per percentage increase in LGE extent in HCM patients with extensive LGE (>15%). While instead of LGE extent, the subendocardium-involved LGE pattern is related to the adverse outcomes in patients with non-extensive LGE (<15%), especially for heart failure-related outcomes. RVIP LGE is commonly seen in HCM, but this LGE location does not merit a prognostic value. Given the prognostic value of extensive LGE has been broadly recognized, subendocardial involvement as an underrecognized LGE pattern shows the potential to improve risk stratification in HCM patients with non-extensive LGE.Acknowledgements
N/AReferences
1. Maron BJ. Clinical Course and Management of Hypertrophic Cardiomyopathy. N Engl J Med. 2018;379:655-668.
2. Maron BJ, Desai MY, Nishimura RA, Spirito P, Rakowski H, Towbin JA, et al. Management of hypertrophic cardiomyopathy: JACC state-of-the-art review. J Am Coll Cardiol. 2022;79:390-414.
3. Mentias A, Raeisi-Giglou P, Smedira NG, Feng K, Sato K, Wazni O, et al. Late Gadolinium Enhancement in Patients With Hypertrophic Cardiomyopathy and Preserved Systolic Function. J Am Coll Cardiol. 2018;72:857-870.
4. Moon JC, McKenna WJ, McCrohon JA, Elliott PM, Smith GC, Pennell DJ. Toward clinical risk assessment in hypertrophic cardiomyopathy with gadolinium cardiovascular magnetic resonance. Journal of the American College of Cardiology. 2003;41:1561-7.
5. Maron MS, Appelbaum E, Harrigan CJ, Buros J, Gibson CM, Hanna C, et al. Clinical profile and significance of delayed enhancement in hypertrophic cardiomyopathy. Circ Heart Fail. 2008;1:184-91.
6. Freed BH, Gomberg-Maitland M, Chandra S, Mor-Avi V, Rich S, Archer SL, et al. Late gadolinium enhancement cardiovascular magnetic resonance predicts clinical worsening in patients with pulmonary hypertension. J Cardiovasc Magn Reson. 2012;14:11.
Figures