4709
The Evaluation of Treatment Effects on Left Ventricular Structure and Function in Primary Aldosteronism by Cardiac Magnetic Resonance Imaging1Department of Radiology, West China Hospital, Sichuan University, Chengdu, China, 2MR Application Predevelopment, Siemens Healthcare GmbH, Erlangen, Germany, 3MR Collaboration, Siemens Healthineers Ltd, Shanghai, China, 4West China Hospital, Sichuan University, Chengdu, China
Synopsis
Keywords: Myocardium, Cardiovascular, cardiac magnetic resonance imaging; left ventricle; primary aldosteronism; strain; dysfunction
This study used routine cardiac function parameters and strain parameters based on cardiac magnetic resonance imaging to evaluate the effects of specific treatments on left ventricular structure and function in patients with PA. We found that patients with PA had lower LV volumes and myocardial mass, as well as improved circumferential and longitudinal myocardial motion both after adrenalectomy and drug treatment. Specific treatment in patients of PA can not only effectively relieve the clinical symptoms, but also improve left ventricular structure and subclinical dysfunction.Introduction
Primary aldosteronism (PA) is caused by renin-independent aldosterone production and is associated with hypertension and increased risk of adverse cardiovascular outcomes1. Previous study demonstrated that patients with PA exhibited greater left ventricular (LV) hypertrophy and enlargement, as well as dysfunction than patients with essential hypertension2, 3. Although specific PA treatment reduces LV myocardial mass and improves LV enlargement4-6, the reversibility of LV dysfunction in patients with PA after treatment is inconclusive7-10. Echocardiography was widely used for the evaluation of the treatment effects on LV structure and function in patients with PA for the convenience of operation,while it was limited by personal manipulation, low signal-to-noise ratio and poor acoustic window, which may reduce the accuracy of measurements11.Cardiac magnetic resonance (CMR) is considered as the reference standard for the assessment of ventricular structure and function12. Therefore, in this study, we aimed to evaluate the left ventricular structure and function in patients with PA using cardiac magnetic resonance (CMR) imaging before and after treatment by adrenalectomy or PA-specific drug treatment.Methods
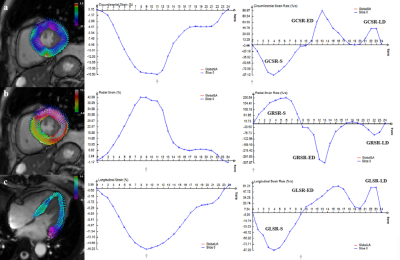
Thirty patients with PA (Female: Male, 22: 8; age, 48±11years) diagnosed at our hospital were prospectively enrolled and were performed CMR cine imaging. Thirteen patients of them received adrenalectomy and the other 17 cases received drug treatment. Furthermore, all of them underwent follow-up CMR median 12 months after specific treatment. Routine cardiac function parameters was analyzed by Argus workstation and strain parameters was analyzed by Trufi-Strain version 2.1 as Figure 1. The paired t-test or Wilcoxon signed rank sum test was used to compare the differences between PA at baseline and after treatment for the routine cardiac function parameters and strain parameters.Results
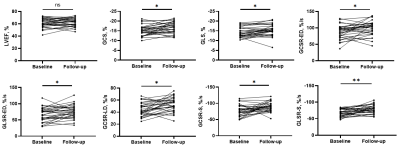
After specific treatment, blood pressure, aldosterone and aldosterone-renin ratio in patients with PA were significantly lower than those at baseline, and the level of serum potassium and renin concentration were significantly higher than those at baseline (all P<0.01). At follow-up, left ventricular end-diastolic volume index (LVEDVI; P<0.001), left ventricular end-systolic volume index (LVESVI; P<0.001) and mass index (LVMI; P<0.001) decreased significantly from at baseline in the patients with PA. Left ventricular ejection fraction (LVEF) values did not show any statistically significant differences (Figure 2). However, after treatment, patients with PA showed significantly increased global circumferential strain (GCS; P=0.003), global longitudinal strain (GLS; P=0.008), global circumferential strain rate-early diastolic (GCSR-ED; P=0.011), global longitudinal strain rate-early diastolic (GLSR-ED; P=0.007), global circumferential strain rate-late diastolic (GCSR-LD; P=0.001)global circumferential strain rate-systolic (GCSR-S; P=0.004), and global longitudinal strain rate-systolic (GLSR-S; P<0.001) compared with those at baseline (Figure 2). When analyzing adrenalectomy and drug treatment separately, LVEDVI, LVEDSVI, LVMI decreased (all P<0.05) and GLSR-S (both P<0.05) improved both after adrenalectomy and drug treatment in patients with PA.Discussion
In the present study, we measured the traditional cardiac function and strain parameters based on CMR to evaluate the effects of specific treatments on cardiac structure and function in patients with PA. Our results showed that treatment by adrenalectomy or drugs reduced the LV cavity and LV mass in the patients with PA while improving serum potassium and blood pressure. Furthermore, although there was no significant change in LVEF, the circumferential and longitudinal myocardial motion in the patients with PA was improved both after adrenalectomy and drug treatment.Conclusion
Specific treatment in patients of PA can not only effectively relieve the clinical symptoms, but also improve left ventricular enlargement and hypertrophy, as well as subclinical dysfunction.Acknowledgements
No acknowledgement found.References
1. Brown JM, Siddiqui M, Calhoun DA, et al. The Unrecognized Prevalence of Primary Aldosteronism: A Cross-sectional Study. Ann Intern Med 2020;173(1):10-20.
2. Zhou F, Wu T, Wang W, et al. CMR-Verified Myocardial Fibrosis Is Associated With Subclinical Diastolic Dysfunction in Primary Aldosteronism Patients. Front Endocrinol (Lausanne) 2021;12:672557.
3. Wu T, Ren Y, Wang W, et al. Left Ventricular Remodeling in Patients with Primary Aldosteronism: A Prospective Cardiac Magnetic Resonance Imaging Study. Korean J Radiol 2021;22(10):1619-1627.
4. Liao CW, Lin YT, Wu XM, et al. The relation among aldosterone, galectin-3, and myocardial fibrosis: a prospective clinical pilot follow-up study. J Investig Med 2016;64(6):1109-13.
5. Lin YH, Wu XM, Lee HH, et al. Adrenalectomy reverses myocardial fibrosis in patients with primary aldosteronism. J Hypertens 2012;30(8):1606-13.
6. Lin YH, Lee HH, Liu KL, et al. Reversal of myocardial fibrosis in patients with unilateral hyperaldosteronism receiving adrenalectomy. Surgery 2011;150(3):526-33.
7. Chen YL, Xu TY, Xu JZ, et al. A Prospective Comparative Study on Cardiac Alterations After Surgery and Drug Treatment of Primary Aldosteronism. Front Endocrinol (Lausanne) 2021;12:770711.
8. Chang YY, Liao CW, Tsai CH, et al. Left Ventricular Dysfunction in Patients With Primary Aldosteronism: A Propensity Score-Matching Follow-Up Study With Tissue Doppler Imaging. J Am Heart Assoc 2019;8(22):e013263.
9. Indra T, Holaj R, Štrauch B, et al. Long-term effects of adrenalectomy or spironolactone on blood pressure control and regression of left ventricle hypertrophy in patients with primary aldosteronism. J Renin Angiotensin Aldosterone Syst 2015;16(4):1109-17.
10. Holaj R, Rosa J, Zelinka T, et al. Long-term effect of specific treatment of primary aldosteronism on carotid intima-media thickness. J Hypertens 2015;33(4):874-82; discussion 882.
11. Bai AD, Steinberg M, Showler A, et al. Diagnostic Accuracy of Transthoracic Echocardiography for Infective Endocarditis Findings Using Transesophageal Echocardiography as the Reference Standard: A Meta-Analysis. J Am Soc Echocardiogr 2017;30(7):639-646.e8.
12. Barison A, Baritussio A, Cipriani A, et al. Cardiovascular magnetic resonance: What clinicians should know about safety and contraindications. Int J Cardiol 2021;331:322-328.
Figures