4705
Right ventricular strain for the diagnosis and prognosis of arrhythmogenic right ventricular cardiomyopathy1Fuwai Hospital, National Center for Cardiovascular Diseases, State Key Laboratory of Cardiovascular, Beijing, China
Synopsis
Keywords: Cardiomyopathy, Quantitative Imaging, arrhythmogenic right ventricular cardiomyopathy
To find out the values of strain parameters in the diagnosis and prognosis of arrhythmogenic right ventricular cardiomyopathy (ARVC), 247 patients with initial diagnosis of suspected ARVC were included in this study. Results showed that right ventricular global longitudinal strain (RV GLS) had moderate to high discriminatory power to identify patients with different likelihood of ARVC. Besides, patients with reduced RV GLS had a higher estimated cumulative incidence of combined cardiovascular events. These findings indicate that cardiac magnetic resonance feature tracking could potentially be used as a preferred imaging method in the first visit and follow-up of ARVC.
Introduction
As an ideal method to assess ventricular volume and function independently of geometric assumptions1,2, cardiovascular magnetic resonance (CMR) plays an important role in the diagnosis of arrhythmogenic right ventricular cardiomyopathy (ARVC) for assessing the structural and functional abnormalities of right ventricle (RV). Quantitative parameters including right ventricular ejection fraction (RVEF) and right ventricular end-diastolic volume index (RVEDVi) measured by CMR are now used as part of the diagnostic criteria3. Whereas, there are still limitations for these conventional parameters. The measurements of RVEF and RVEDVi are time-consuming and conventional parameters are insensitive in detecting subtle motion abnormalities in early disease4,5. Currently, CMR feature-tracking (CMR-FT) has been introduced as a convenient and more sensitive method in the quantitative evaluation of myocardial function to recognize functional changes even before the decrease of ejection fraction6,7. In ARVC, there are few studies on the strain characteristics of the entire modified Task Force Criteria (mTFC) diagnosed population3 that consist of patients with ‘possible’, ‘borderline’ and ‘definite’ ARVC, and the specific diagnostic value of strain parameters are still undetermined. Therefore, based on a large cohort of patients with initial diagnosis of suspected ARVC, we aim to (1) demonstrate the myocardial strain characteristics of patients with mTFC diagnosed ARVC and find out the optimal strain parameter to assist the diagnosis; and to (2) verify the value of strain in the prognosis of the patients.Method
In this retrospective observational cohort study, 247 mTFC diagnosed ARVC patients and 40 healthy controls were enrolled for analysis. Patients were divided into ‘possible’, ‘borderline’ and ‘definite’ ARVC based on their family history, cardiovascular magnetic resonance (CMR), electrocardiogram, Holter monitoring and endomyocardial biopsy. Primary outcome was defined as a composite of cardiovascular events including cardiovascular death, heart transplantation, and sustained ventricular tachycardia. One-way analysis of variance (ANOVA) and Kruskal- Wallis tests (with post-hoc analysis using Bonferroni correction) were used for comparison among different diagnostic groups based upon the variables and data distribution. And we performed univariate and multivariate Cox proportional hazards regression analysis to estimate the hazard of primary end points for each risk factors.Results
Of the 247 included patients (median age 38, IQR 28-48, 167 men), there were 25 patients with possible ARVC, 40 patients with borderline ARVC and 182 patients with definite ARVC according to mTFC. Patients group showed significant larger biventricular volume and lower biventricular systolic function than controls (all p<0.01). In the comparison among different diagnostic groups, only right ventricular parameters differed significantly. Patients with definite ARVC had significantly reduced RV global circumferential (GCS), radial (GRS) and longitudinal strain (GLS) than possible and borderline ARVC patients (all p<0.001). On ROC analysis, RV GLS was a stronger discriminator between patient group and healthy controls than RV GCS and RV GRS [area under the curve (AUC): 0.88 vs. 0.82 and 0.84]. Patients with ‘possible’ or ‘borderline’ diagnosis were defined as ‘suspected’ ARVC. RV GLS showed moderate discriminatory power to identify ‘suspected’ ARVC (AUC: 0.73) and high discriminatory power to identify ‘definite’ ARVC (AUC: 0.93). The best cut-off values for RV GLS to identify ‘suspected’ ARVC patients and ‘definite’ ARVC patients were -20.02% (sensitivity of 64.62% and specificity of 81.58%) and -17.32% (sensitivity of 81.32 and specificity of 92.11) respectively. During 3.3 (IQR 1.9-4.8) years of follow-up, 28% of patients experienced combined cardiovascular events. Multivariable analysis showed that patients with RV GLS ≥-17.32% had a higher risk of combined cardiovascular events (Hazard Ratio, 2.11[1.10-4.04]; p=0.03).Conclusion
As a reproducible and easily accessible quantitative parameter to assess right ventricular dysfunction, CMR-FT derived RV GLS might provide a new insight into the diagnosis of ARVC. Furthermore, we recognize RV GLS as a novel parameter to predict combined cardiovascular events, combined with which the clinical value of CMR-FT in ARVC is further confirmed.Acknowledgements
This study was co-funded by the National Natural Science Foundation of China (No. 81930044) and National Key Research and Development Program of China (No.2021YFF0501404, 2021YFF0501400).
References
1. Gandjbakhch E, Redheuil A, Pousset F, et al. Clinical Diagnosis, Imaging, and Genetics of Arrhythmogenic Right Ventricular Cardiomyopathy/Dysplasia: JACC State-of-the-Art Review. Journal of the American College of Cardiology. 2018;72(7):784-804.
2. Mooij CF, de Wit CJ, Graham DA, et al. Reproducibility of MRI measurements of right ventricular size and function in patients with normal and dilated ventricles. Journal of magnetic resonance imaging: JMRI. 2008;28(1):67-73.
3. Marcus FI, McKenna WJ, Sherrill D, et al. Diagnosis of arrhythmogenic right ventricular cardiomyopathy/dysplasia: proposed modification of the Task Force Criteria. European heart journal. Apr 2010;31(7):806-14.
4. Mast TP, Taha K, Cramer MJ, et al. The Prognostic Value of Right Ventricular Deformation Imaging in Early Arrhythmogenic Right Ventricular Cardiomyopathy. JACC Cardiovascular imaging. 2019;12(3):446-455.
5. Vigneault DM, te Riele AS, James CA, et al. Right ventricular strain by MR quantitatively identifies regional dysfunction in patients with arrhythmogenic right ventricular cardiomyopathy. Journal of magnetic resonance imaging: JMRI. May 2016;43(5):1132-9.
6. Geva T. Imaging criteria for arrhythmogenic right ventricular cardiomyopathy: an incomplete journey. Journal of the American College of Cardiology. 2015;65(10):996-998.
7. Kalam K, Otahal P, Marwick TH. Prognostic implications of global LV dysfunction: a systematic review and meta-analysis of global longitudinal strain and ejection fraction. Heart (British Cardiac Society). 2014;100(21):1673-1680.
Figures
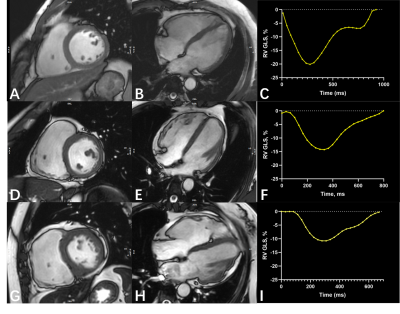
The top line shows the images of a 38-year-old male with possible diagnosis of ARVC according to mTFC. Images in the second line come from a 30-year-old male with borderline diagnosis. The bottom column demonstrates the images of a 44-year-old female with definite ARVC. (A), (D) and (G), cine images in short-axis view; (B), (E) and (H), cine images in 4-chamber view; (C), (F) and (I), RV GLS in the whole cardiac cycle. GLS, global longitudinal strain; ARVC, arrhythmogenic right ventricular cardiomyopathy; mTFC, modified Task Force Criteria.
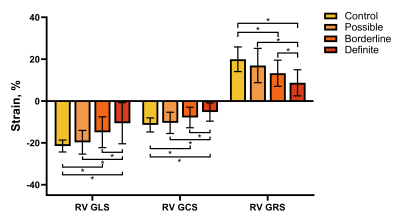
Comparison of right ventricular strain parameters among different diagnostic groups. RV strain parameters derived from CMR-FT reduced with the likelihood of ARVC. RV, right ventricle; CMR, cardiovascular magnetic resonance; FT, feature tracking; GLS, global longitudinal strain; GCS, global circumferential strain; GRS, global radial strain. Statistically significant differences are indicated by * on the bar graph.
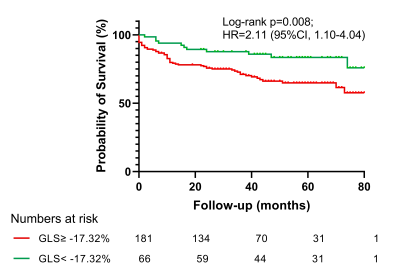
Kaplan-Meier survival analysis showed patients with RV GLS ≥-17.32% had a higher estimated cumulative incidence of combined cardiovascular events. P-value was calculated using log-rank test. RV, right ventricle; GLS, global longitudinal strain.