4694
Early evaluation of subclinical cardiotoxicity in HER2-positive breast cancer patients with low-moderate cardiovascular risk using MRI
Sainan Cheng1, Jianwei Wang1, Yawen Wang1, Linlin Qi1, Fenglan Li1, Jianing Liu1, Jiaqi Chen1, Yang Fan2, and Lizhi Xie2
1Department of Diagnostic Radiology, National Cancer Center/ Cancer Hospital, Chinese Academy of Medical Sciences and Peking Union Medical College, Beijing, China, 2MR Research China, GE Healthcare, Beijing, China
1Department of Diagnostic Radiology, National Cancer Center/ Cancer Hospital, Chinese Academy of Medical Sciences and Peking Union Medical College, Beijing, China, 2MR Research China, GE Healthcare, Beijing, China
Synopsis
Keywords: Heart, Cardiovascular, cardiotoxicity
This study explored the early cardiac changes in HER2-positive patients treated with HER2-targeted or anthracycline therapy through cardiac MRI. The results showed frequent signs of subclinical cardiotoxicity after short-term anti-cancer therapy, despite with low-moderate cardiovascular risk. T1 mapping showed the capability for early detection of pathological myocardial changes before cardiac contractile dysfunction. In HER2-positive breast cancer patients, cardiotoxicity surveillance is important and should be carefully done even with low-moderate cardiovascular risk, especially for those received anthracycline-based therapy.Introduction
Advances in breast cancer therapy, including the development of targeted therapies, have been associated with improved prognosis in HER2-positive breast cancer patients. Despite the impressive anticancer benefit, the frequently cardiotoxicity due to cancer therapy limits their clinical use and may reduce the quality of life of cancer survivors[1]. Early identification of cardiotoxicity may play a pivotal role in avoiding treatment interruption and improving quality of life[2]. However, cardiac surveillance during cancer therapies is easily overlooked in patients with low cardiovascular risk at baseline, especially for those received non-anthracycline-based HER2-targeted therapy. In prior studies, cardiovascular risk stratification of HER2-positive breast cancer participants was not conducted at baseline. Data on early cardiac changes after a short-term anti-cancer therapy in HER2-positive breast cancer patients with low-moderate cardiovascular risk was limited. Therefore, the purpose of this study was to explore the early cardiac changes in HER2-positive patients with low-moderate cardiovascular risk through cardiac MRI. In addition, because anthracycline is a risk factor for HER2-targeted therapy, patients treated with HER2-targeted therapy and anthracycline therapy were compared for further understand the cardiotoxicity induced by HER2-targeted therapy.Methods
We conducted a prospective cohort study of newly diagnosed HER2-positive breast cancer patients. Patients were divided into two groups according to chemotherapy regimen: HER2-targeted therapy group (treated with trastuzumab or plus pertuzumab without anthracycline) and anthracycline chemotherapy group. Cardiac MRIs (SIGNA Architect, GE Healthcare, Waukesha, WI, USA) were done before treatment and 3 months after starting, covering ventricular volumes, cardiac function, systolic myocardial strain, myocardial oedema, T1 and T2 relaxation times. The paired t test or Wilcoxon signed-rank test was used for intraindividual comparisons. The unpaired t test or Mann‒Whitney U test was used to compare variables between subgroups.Results
Thirty-one HER2–positive breast cancer patients were evaluated (21 in the HER2-targeted therapy group, 10 in the anthracycline chemotherapy group) (Table 1). 94% patients were at low cardiovascular toxicity risk. 7 (23%) patients developed mild asymptomatic cancer therapy–related cardiac dysfunction (CTRCD) at follow-up. Patients displayed decreased left ventricular (LV) systolic function (LV ejection fraction, cardiac output index, stroke volume index and strain parameters), increased T1 and T2 relaxation times and increased LV end systolic volume index at follow-up (p<0.05) (Table 2 and Figure 1). There was no significant difference of CTRCD between anthracycline chemotherapy group and HER2-targeted therapies group. However, T1 relaxation time and heart rate was significantly higher in anthracycline chemotherapy group than in HER2-targeted therapies group at follow-up (p<0.05), while there were on significant differences regarding T1 relaxation time and heart rate between two groups at baseline (Table 3).Discussion
This study focused on HER2-positive breast cancer patients with low-moderate cardiovascular risk. The results showed that subclinical CTRCD after a short-term therapy was frequent in this group (23%). Its overall incidence is highly variable in previous studies, ranging from 7.6% to 28%[3-6]. The majority of participants in previous studies received sequential anthracycline and trastuzumab. Thus, it can be seen that subclinical CTRCD is still frequent in HER2-positive breast cancer patients received anthracycline or HER2-targeted therapies, even with low-moderate cardiovascular risk. Consistent with previous findings[7, 8], patients showed a significant increase in T1 and T2 relaxation times at follow-up compared with baseline, which may reflect myocardial injury during cancer therapy.Although anthracycline might be associated with a higher rate of left ventricular dysfunction[9], we found no significant differences of LV ejection fraction or strain parameters between two groups at baseline or follow-up. However, for subgroup analysis, T1 relaxation times were significantly higher in patients treated with anthracycline chemotherapy than those with HER2-targeted therapy. T1 mapping, one of the tissue-characterization techniques, enables detecting early pathological myocardial changes before cardiac contractile dysfunction.
Conclusion
For patients with HER2-positive breast cancer, Cardiac MRI scans showed frequent signs of subclinical cardiotoxicity after a short-term anti-cancer therapy, despite with low-moderate cardiovascular risk. The incidence of CTRCD was not significantly different between patients treated with non- anthracycline-based HER2-targeted therapy and anthracycline therapy, but T1 relaxation time was significantly higher after anthracycline therapy.Acknowledgements
No acknowledgement found.References
1. Herrmann J. Adverse cardiac effects of cancer therapies: cardiotoxicity and arrhythmia. Nat Rev Cardiol 2020, 17(8): 474-502.2. Lyon AR, Lopez-Fernandez T, Couch LS, Asteggiano R, Aznar MC, Bergler-Klein J, et al. 2022 ESC Guidelines on cardio-oncology developed in collaboration with the European Hematology Association (EHA), the European Society for Therapeutic Radiology and Oncology (ESTRO) and the International Cardio-Oncology Society (IC-OS). Eur Heart J Cardiovasc Imaging 2022, 23(10): e333-e465.
3. Tarantini L, Cioffi G, Gori S, Tuccia F, Boccardi L, Bovelli D, et al. Trastuzumab adjuvant chemotherapy and cardiotoxicity in real-world women with breast cancer. J Card Fail 2012, 18(2): 113-119.
4. Bouwer NI, Liesting C, Kofflard MJM, Brugts JJ, Kock MCJ, Kitzen J, et al. 2D-echocardiography vs cardiac MRI strain: a prospective cohort study in patients with HER2-positive breast cancer undergoing trastuzumab. Cardiovasc Ultrasound 2021, 19(1): 35.
5. Lidbrink E, Chmielowska E, Otremba B, Bouhlel A, Lauer S, Liste Hermoso M, et al. A real-world study of cardiac events in > 3700 patients with HER2-positive early breast cancer treated with trastuzumab: final analysis of the OHERA study. Breast Cancer Res Treat 2019, 174(1): 187-196.
6. Esmaeilzadeh M, Urzua Fresno CM, Somerset E, Shalmon T, Amir E, Fan CS, et al. A Combined Echocardiography Approach for the Diagnosis of Cancer Therapy-Related Cardiac Dysfunction in Women With Early-Stage Breast Cancer. JAMA Cardiol 2022, 7(3): 330-340.
7. Giusca S, Korosoglou G, Montenbruck M, Gersak B, Schwarz AK, Esch S, et al. Multiparametric Early Detection and Prediction of Cardiotoxicity Using Myocardial Strain, T1 and T2 Mapping, and Biochemical Markers: A Longitudinal Cardiac Resonance Imaging Study During 2 Years of Follow-Up. Circ Cardiovasc Imaging 2021, 14(6): e012459.
8. Terui Y, Sugimura K, Ota H, Tada H, Nochioka K, Sato H, et al. Usefulness of cardiac magnetic resonance for early detection of cancer therapeutics-related cardiac dysfunction in breast cancer patients. International Journal of Cardiology 2022.
9. Greenlee H, Iribarren C, Rana JS, Cheng R, Nguyen-Huynh M, Rillamas-Sun E, et al. Risk of Cardiovascular Disease in Women With and Without Breast Cancer: The Pathways Heart Study. Journal of Clinical Oncology 2022, 40(15): 1647-1658.
Figures
*Data are given as means ± standard deviations.
†Data in parentheses are percentages.
BMI = body mass index; HFA-ICOS = Heart Failure Association-International Cardio-Oncology Society; HER2=human epidermal growth factor receptor 2
†Data in parentheses are percentages.
BMI = body mass index; HFA-ICOS = Heart Failure Association-International Cardio-Oncology Society; HER2=human epidermal growth factor receptor 2
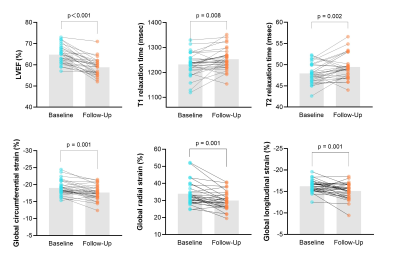
Bar graphs show changes in cardiac MRI variables between the baseline and follow-up MRI examinations. Bars represent median LVEF in the first graph and represent mean data in other graphs. Blue plots represent intraindividual values at baseline, and orange plots represent intraindividual values at the follow-up MRI.
Data are given as means ± standard deviations or medians with interquartile ranges in parentheses. LV = left ventricular.
Data are given as means ± standard deviations or medians with interquartile ranges in parentheses. LV = left ventricular.
DOI: https://doi.org/10.58530/2023/4694