4689
The evaluation of short- and mid-term effects of sleeve gastrectomy on left ventricular function in obesity: a prospective CMR study1Department of Radiology, West China Hospital, Sichuan University, Chengdu, China
Synopsis
Keywords: Heart, Myocardium, obesity; left ventricular function; cardiac magnetic resonance
This study investigate left ventricular function of obese patients with no known heart disease who underwent laparoscopic sleeve gastrectomy (LSG) by cardiac magnetic resonance (CMR) in their short- and mid-term postoperative follow-up. We found that obese patients who underwent LSG had a significant decrease in body weight, left ventricular mass and left ventricular cavity in the short- and mid- term postoperative. In the mid-term postoperative, the left ventricular subclinical systolic dysfunction of left ventricle significantly improved.Introduction
Obesity is one of the main risk factors of cardiovascular disease and has become a major challenge to population health in China1. Previous studies have demonstrated that obesity can lead to enlargement of left ventricular (LV) cavity, increase of LV mass, and even cause LV dysfunction2, 3. Laparoscopic sleeve gastrectomy (LSG) is one of the most effective treatments for severe obesity. Cardiovascular magnetic resonance (CMR) imaging is considered as the reference standard for the evaluation of cardiac structure and function4. Cardiac magnetic resonance feature tracking can quantitatively evaluate the early changes of global and local myocardial motion function with good reproducibility5. Studies demonstrating the positive effect of bariatric surgery on cardiovascular morphology and structure had been conducted6, 7. However, there was no study examining the impacts of bariatric surgery on subclinical dysfunction of left ventricular functions using CMR. Therefore, this study aimed to investigate left ventricular function of obese patients with no known heart disease who underwent LSG by CMR in their short- and mid-term postoperative follow-up.Methods
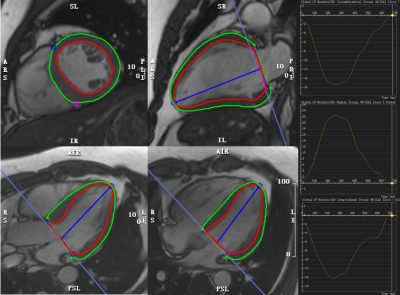
Thirty-three obese patients (Male: Female, 11: 22; age, 30±8years) without known heart disease who had undergone LSG at our hospital from January 2020 to January 2021 were prospectively enrolled. All patients underwent CMR cine imaging before operation, 1 and 6 months after operation. All CMR examinations were performed on a 3.0 T scanner (MAGNETOM Skyra, Siemens Healthcare, Erlangen, Germany). The protocol included electrocardiography-gated balanced steady state free precession images of long-axis two-, three- and four-chamber views as well as short-axis stacks. CVI 42 was used to analyse cine images to obtain routine cardiac function parameters and strain parameters (Figure 1). The Shapiro-Wilk test was used to analyze the normal distribution of continuous variables. For the purpose of comparing consecutive measurements, the repeated-measures ANAVA or Friedman test was employed. For post hoc analysis, the paired t test or Wilcoxon signed-rank test was used.Results
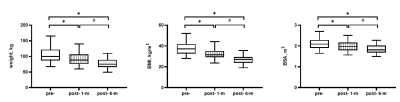
After LSG, the body weight, body mass index (BMI), body surface area (BSA) of obese patients decreased significantly (all P<0.001; Figure 2). At 1 and 6 months postoperative, left ventricular end-diastolic volume (LVEDV), left ventricular mass (LVMASS) and LVMASS/BSA were significantly lower than those at preoperative (all P<0.05), and LVESV at 6 months postoperative was significantly lower than that at preoperative and 1 month postoperative (both P<0.05). There was no significant difference in left ventricular ejection fraction (LVEF) between preoperative and postoperative (both P>0.05), but LVEF at 6months postoperative was higher than that at 1 month postoperative (P=0.008). At 6 months postoperative,global peak circumferential strain (GCS), global peak radial strain (GRS), and global peak longitudinal strain (GLS) were significantly improved as compared with those at preoperative and 1 month postoperative (all P<0.05; Figure 3).Discussion
In our study, obese patients showed a decrease in LV cavity and mass in the early stage after LSG, and gradually improved with weight loss. In the mid-term after LSG, although LVEF was not significantly improved compared with that at preoperative, the LV circumferential, radial and longitudinal strain were significantly improved. In previous echocardiographic studies, Tuluce et al.8 found that GLS significantly improved 1 month after LSG; while in Inci et al.9 observed that GLS showed no changes at 1 month postoperative, but GLS improved at 6 months postoperative. However, because acoustic windows become more limited as the body weight increases, echocardiography may have reduced accuracy in patients with obesity. Our CMR study suggested that circumferential, radial and longitudinal subclinical systolic dysfunction improved in obese patients in the mid-term after LSG.Conclusion
Obese patients who underwent LSG had a significant decrease in body weight, left ventricular mass and left ventricular cavity in the short- and mid- term postoperative. In the mid-term postoperative, the left ventricular subclinical systolic dysfunction of left ventricle significantly improved.Acknowledgements
No acknowledgement found.References
1. Zeng Q, Li N, Pan XF, et al. Clinical management and treatment of obesity in China. Lancet Diabetes Endocrinol 2021;9:393-405
2. Liu J, Li J, Pu H, et al. Cardiac remodeling and subclinical left ventricular dysfunction in adults with uncomplicated obesity: a cardiovascular magnetic resonance study. Quant Imaging Med Surg 2022;12:2035-2050
3. Snelder SM, de Groot-de Laat LE, Biter LU, et al. Subclinical cardiac dysfunction in obesity patients is linked to autonomic dysfunction: findings from the CARDIOBESE study. ESC Heart Fail 2020;7:3726-3737
4. Pattynama PM, De Roos A, Van der Wall EE, et al. Evaluation of cardiac function with magnetic resonance imaging. Am Heart J 1994;128:595-607
5. Ibrahim el SH. Myocardial tagging by cardiovascular magnetic resonance: evolution of techniques--pulse sequences, analysis algorithms, and applications. J Cardiovasc Magn Reson 2011;13:36
6. de Witte D, Wijngaarden LH, van Houten VAA, et al. Improvement of Cardiac Function After Roux-en-Y Gastric Bypass in Morbidly Obese Patients Without Cardiac History Measured by Cardiac MRI. Obes Surg 2020;30:2475-2481
7. Rider OJ, Francis JM, Ali MK, et al. Beneficial cardiovascular effects of bariatric surgical and dietary weight loss in obesity. J Am Coll Cardiol 2009;54:718-726
8. Tuluce K, Kara C, Tuluce SY, et al. Early Reverse Cardiac Remodeling Effect of Laparoscopic Sleeve Gastrectomy. Obes Surg 2017;27:364-375
9. Inci S, Gül M, Alsancak Y, et al. Short- and mid-term effects of sleeve gastrectomy on left ventricular function with two-dimensional speckle tracking echocardiography in obese patients. Echocardiography 2019;36:2019-2025
Figures