4673
Effect of Kaftrio therapy on pulmonary ventilation derived by 3D phase-resolved functional lung MRI in cystic fibrosis patients1Institute of Diagnostic and Interventional Radiology, Hannover Medical School, Hannover, Germany, 2Biomedical Research in Endstage and Obstructive Lung Disease Hannover (BREATH), German Center for Lung Research (DZL), Hannover, Germany, 3MR Application Predevelopment, Siemens Healthcare GmbH, Erlangen, Germany, 4Department for Pediatric Pneumology, Allergology and Neonatology, Hannover Medical School, Hannover, Germany
Synopsis
Keywords: Lung, Lung
Kaftrio therapy was shown to improve global clinical ventilation parameters in cystic fibrosis (CF) patients. 3D phase-resolved functional lung (PREFUL) MRI offers a contrast-free assessment of pulmonary ventilation during free breathing. The aim of this study was to determine whether 3D PREFUL parameters are suitable to measure response to Kaftrio therapy and their association with clinical outcomes in CF patients. All assessed MRI and clinical parameters significantly improved after initiation of Kaftrio. Relative change between baseline and post-treatment scans of 3D PREFUL ventilation defect percentage maps was in agreement with forced expiratory volume in 1 second and lung clearance index.Introduction
Triple CFTR-modulator therapy with Kaftrio (elexacaftor/tezacaftor/ivacaftor) was shown to improve global clinical ventilation parameters and the semi-quantitative morphologic MRI scoring in cystic fibrosis (CF) patients1. 3D phase-resolved functional lung (PREFUL) MRI is a promising technique, which enables quantitative assessment of pulmonary ventilation during free breathing on a regional level of the total lung volume2. 3D PREFUL ventilation parameters have been shown to correlate well with spirometric measurements and showed a good interscan reproducibility in a study cohort consisting of healthy volunteers and chronic obstructive pulmonary disease patients3. However, it is unknown whether 3D PREFUL parameters are sensitive to measure treatment changes in patients with CF. The objective of this study was to investigate if the ventilation parameters derived by 3D PREFUL are suitable to measure response to Kaftrio therapy in comparison to clinical outcome measures in CF patients.Methods
23 CF patients (13 female, age range: 13-46 years) underwent MRI on a 1.5T (MAGNETOM Avanto; Siemens Healthcare, Erlangen, Germany), spirometry and multiple breath washout (MBW) at baseline and 11-28 weeks after initiation of Kaftrio therapy. In addition to morphological sequences as described before1, an eight-minute 3D PREFUL measurement2 was used to assess regional lung ventilation. The following sequence parameters were used for the 3D PREFUL: TE 0.81 ms, TR 1.9 ms, flip angle 3.5°, FOV 45 x 45 cm2, matrix size 112 x 112 interpolated to 224 x 224, 52-60 partitions, 6/8 partial Fourier along the partition dimension, pixel bandwidth 1500 Hz/pixel, slice thickness 4 mm interpolated to 2 mm.Morphological MR images were evaluated using MRI, based on a well-established semi-quantitative scoring system4(including global, morphology, perfusion, wall thickening / bronchiectasis, mucus and abscesses / sacculations score).
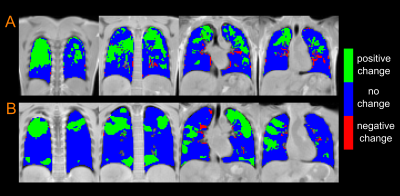
After successful 3D PREFUL image reconstruction of ~40 breathing phases, all respiratory resolved images were registered towards end-inspiration image using a software package, developed by Daniel Forsberg5. Using 3D PREFUL registered images, ventilation defect percentage (VDP) maps derived from static regional ventilation (RVent)6 and dynamic cross-correlation (CC)7 maps based on previously published thresholds were calculated3. To analyze the treatment effect on regional level, morphological images of the second visit were co-registered to the morphological end-inspiratory image of the first visit. The treatment response maps (TRMs) were then calculated by subtracting the VDP map after therapy from the baseline VDP maps. Post-treatment improved ventilation volume (IVVRVent and IVVCC) was calculated as a number of positively changed voxels in TRMs multiplied by lung volume in ml. Both volumes were normalized to body surface area (BSA).
Spirometry outcomes (forced expiratory volume in 1 second (FEV1) and forced expiratory flow at 25% (FEF25) of forced vital capacity) were obtained according to ATS/ERS guidelines8 and analyzed with GLI reference values9. Lung clearance index (LCI) was assessed using the nitrogen MBW technique according to ATS/ERS guidelines10.
Parameters are shown as mean values (standard deviation). The treatment effect on all derived parameters was analyzed using a paired Wilcoxon signed rank test. Treatment changes and post-treatment agreement between 3D PREFUL and clinical parameters were evaluated using Spearman correlation (r) analysis.
Results
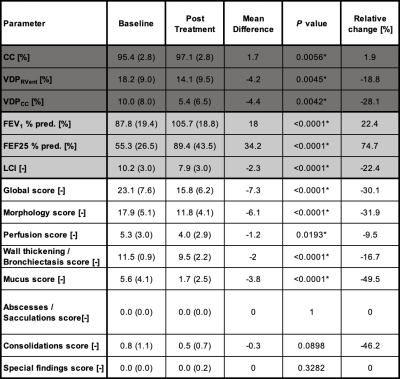
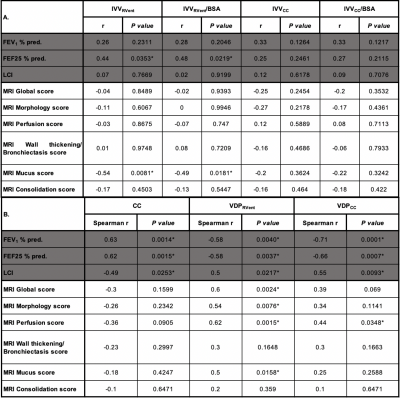
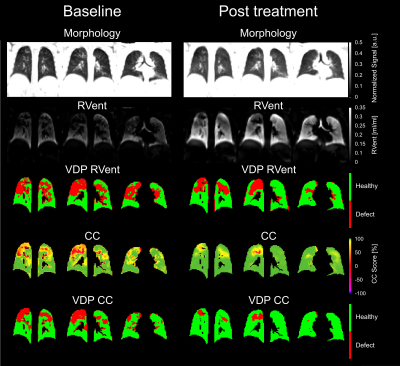
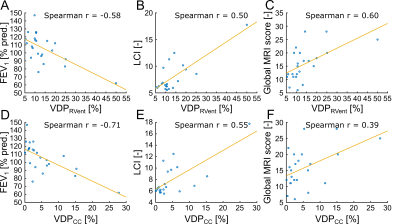
Therapy with Kaftrio significantly improved all ventilation markers derived by 3D PREFUL MRI (all P<0.0056, Table 1) as well as MRI global, morphology and perfusion scores (all P<0.02, Table 1). Also FEV1 and LCI significantly improved after therapy (all P<0.0001, Table 1). Representative 3D PREFUL ventilation parameters at baseline and post Kaftrio treatment are depicted in Figure 1.There was no significant correlation between absolute and relative treatment changes of 3D PREFUL MRI ventilation parameters (CC, VDPRVent and VDPCC) with FEV1, LCI, MRI scores (P>0.05). Figure 3 shows regional TRMs derived by 3D PREFUL for two study participants. Looking only at positive changes in TRMs, the IVVRVent and IVVRVent normalized to BSA were significantly correlated to relative treatment changes of FEF25 and mucus MRI score (all |r|>0.44, all P<0.0353, Table 2A). In post-treatment analysis, 3D PREFUL derived VDP values significantly correlated with spirometry, LCI, global score, morphology score and perfusion score (all |r|>0.44, all P<0.0348, Table 2B, Figure 2), except for correlation of VDPCC with global and morphology score. CC values derived by 3D PREFUL correlated significantly with FEV1, FEF25 and LCI (all |r|>0.49, all P<0.0253, Table 2B).
Discussion
3D PREFUL MRI derived VDP maps show significantly reduced ventilation defects (19-28%) after Kaftrio therapy.The significant post treatment correlations of 3D PREFUL ventilation measures especially with LCI, FEV1 % pred., and global MRI score suggest that 3D PREFUL MRI is sensitive to measure improved regional ventilation of the lung parenchyma due to reduced inflammation induced by Kaftrio therapy in CF patients. Regarding relative treatment change, there was significant correlation of 3D PREFUL MRI derived improved ventilation volume (IVVRVent and IVVRVent normalized to BSA) with relative change of FEF25 and mucus MRI score. This may show the complementary value of 3D PREFUL MRI to global clinically established measures such as FEV1 and LCI. Future multicentre validation studies are necessary to investigate if 3D PREFUL MRI regional ventilation assessment may add value to current clinical standard techniques as spirometry, MBW, or gas-based MRI techniques.
Conclusion
3D PREFUL ventilation MRI is a very promising tool to monitor regional dynamic ventilation changes in CF patients after Kaftrio therapy.Acknowledgements
This work was funded by the German Center for Lung Research (DZL).References
1. Graeber SY, Renz DM, Stahl M, et al. Effects of Elexacaftor/Tezacaftor/Ivacaftor Therapy on Lung Clearance Index and Magnetic Resonance Imaging in Patients with Cystic Fibrosis and One or Two F508del Alleles. Am J Respir Crit Care Med. May 2022. doi:10.1164/rccm.202201-0219OC
2. Klimeš F, Voskrebenzev A, Gutberlet M, et al. 3D phase‐resolved functional lung ventilation MR imaging in healthy volunteers and patients with chronic pulmonary disease. Magn Reson Med. 2021;85(2):912-925. doi:10.1002/mrm.28482
3. Klimeš F, Voskrebenzev A, Gutberlet M, et al. Repeatability of dynamic 3D phase-resolved functional lung (PREFUL) ventilation MR Imaging in patients with chronic obstructive pulmonary disease and healthy volunteers. J Magn Reson Imaging. 2021;54(2):618-629. doi:10.1002/jmri.27543
4. Eichinger M, Optazaite DE, Kopp-Schneider A, et al. Morphologic and functional scoring of cystic fibrosis lung disease using MRI. Eur J Radiol. 2012;81(6):1321-1329. doi:10.1016/j.ejrad.2011.02.045
5. Forsberg D. fordanic/image-registration (https://github.com/fordanic/image-registration), GitHub. Retrieved September 8, 2021
6. Klimeš F, Voskrebenzev A, Gutberlet M, et al. Free‐breathing quantification of regional ventilation derived by phase‐resolved functional lung (PREFUL) MRI. NMR Biomed. 2019;(February):e4088. doi:10.1002/nbm.4088
7. Voskrebenzev A, Gutberlet M, Klimeš F, et al. Feasibility of quantitative regional ventilation and perfusion mapping with phase-resolved functional lung (PREFUL) MRI in healthy volunteers and COPD, CTEPH, and CF patients. Magn Reson Med. 2018;79(4):2306-2314. doi:10.1002/mrm.26893
8. Miller MR, Hankinson J, Brusasco V, et al. Standardisation of spirometry. Eur Respir J. 2005;26(2):319-338. doi:10.1183/09031936.05.00034805
9. Quanjer PH, Stanojevic S, Cole TJ, et al. Multi-ethnic reference values for spirometry for the 3-95-yr age range: the global lung function 2012 equations. Eur Respir J. 2012;40(6):1324-1343. doi:10.1183/09031936.00080312
10. Robinson PD, Latzin P, Verbanck S, et al. Consensus statement for inert gas washout measurement using multiple- and singlebreath tests. Eur Respir J. 2013;41(3):507-522. doi:10.1183/09031936.00069712
Figures