4509
Assessing Ventilation Dynamics of Lung Transplantation with Free-Breathing Hyperpolarized Xenon-129
Faraz Amzajerdian1, Hooman Hamedani1, Ryan Baron1, Mostafa Ismail1, Luis Loza1, Kai Ruppert1, Stephen Kadlecek1, and Rahim Rizi1
1Radiology, University of Pennsylvania, Philadelphia, PA, United States
1Radiology, University of Pennsylvania, Philadelphia, PA, United States
Synopsis
Keywords: Hyperpolarized MR (Gas), Lung
Regional quantification of ventilation dynamics can provide valuable insights into the functional changes associated with both unilateral and bilateral lung transplantation, potentially improving diagnostic monitoring and providing a better understanding of underlying pathophysiology. By imaging hyperpolarized xenon-129 (HXe) continuously over an extended period of time, ventilation dynamics more representative of steady-state, physiological breathing were derived and used to assess differences between unilateral and bilateral transplant patients.Introduction
Despite the number of patients on the waiting list far exceeding the number of available organs, lung transplantation remains the primary treatment option for many end-stage lung diseases. As a result, unilateral transplant provides many advantages for reducing overall patient mortality, essentially doubling the number of potential transplants per donor, shortening waitlist times, and reducing perioperative complications due to increased surgical simplicity (vs. bilateral transplant)1. While outcomes are generally worse compared to bilateral transplants, the pathophysiology of graft failure is not fully understood in either case. Hyperpolarized xenon-129 (HXe) MRI’s unique ability quantify regional lung function may therefore provide additional insights into post-transplant structural and functional changes relevant to graft health, and could reveal differences in the progression between unilateral and bilateral transplants. In particular, imaging low doses of HXe continuously during normal breathing can provide a better representation of physiological respiratory dynamics compared to imaging during extended breath-holds. In this work, we present initial results from a 4-minute free-breathing protocol in a healthy volunteer and 6 transplant patients.Methods
Subject demographics are shown in Table 1. The left- and right-lung unilateral transplant patients were both initially diagnosed with idiopathic pulmonary fibrosis (IPF) and imaged 3 and 6 months post-surgery, respectively, while the bilateral subjects were imaged between 6 and 24 months post-transplant. Same day pulmonary function testing (PFT) was performed before each imaging session. All imaging was performed with an Institutional Review Board (IRB)-approved protocol in a 1.5T scanner (Magnetom Avanto, Siemens) using an 8-channel 129Xe coil (Stark Contrast, Germany). A prototype commercial system (XeBox-E10, Xemed LLC, NH) was used to polarize 87% enriched xenon-129.Subjects breathed room air spontaneously through a sealed face mask, while a custom gas delivery device administered 50 mL of HXe upon every inhalation. Imaging was performed continuously over approximately 4 minutes (50 breaths, for a total of 2.5L of gas) via an isotropic 3D golden-angle spiral sequence. Parameters included: TR/TE of 7.83/0.62 ms, flip angle of 4°, and field-of-view of 350x350x350 mm3 reconstructed onto an 80x80x80 grid. The lung inflation level was approximated from the center k-space gas signals across the acquisition and used to retroactively gate each spiral interleave into 16 distinct phases of an average breathing cycle. All images were registered to the end-inhale phase using symmetric diffeomorphic normalization and the ANTs toolkit. The time-varying dynamics across each voxel were analyzed to derive tidal volumes (TV), functional residual capacity (FRC), fractional ventilation (FV), and arrival times2.
Results and Discussion
Figure 1 shows a representative coronal slice from both unilateral transplant patients, post-registration, across 8 of the 16 phases illustrating inhalation and exhalation signal dynamics. While gas-phase signal intensity is not necessarily correlated to lung function, the transplanted lung exhibited higher signal and gas concentration compared to the native lung in both subjects. However, this may be more a consequence of donor/recipient size mismatch resulting in asymmetrical filling. Figure 2 shows the TV, FRC, FV, and arrival time maps for the same slice in the same subjects. While the tidal and residual volumes in the transplanted lungs are significantly higher than in the native lungs, the FV, a functional measure of gas turnover, remained fairly homogeneous. The arrival time maps illustrate the time, relative to the gas entering the lungs, that each voxel takes to reach its maximum signal intensity. For both subjects, the transplanted lung was slower to reach this maximum, although it is not apparent whether this is due to the size difference between the lungs or a reflection of post-operative complications prior to recovery.Figure 3 shows the measurement averages in the right and left lung of each subject from anterior-to-posterior, with the dashed lines indicating the native lung for the unilateral transplants. For the healthy subject, the right and left lungs strongly correlate with each other, indicative of the homogenous gas distribution and healthy lung function, especially considering the anterior-to-posterior gravitational gradient apparent in the FV maps. Notably, arrival times are fairly constant across the lungs, with slight deviation at the anterior regions of the lungs most likely due to partial volume effects and asymmetrical lung shape. The unilateral subjects closely resemble each other, with the transplanted lung consistently maintaining higher gas volumes, higher FV, and longer arrival times compared to the native lung. Interestingly, the transplanted lungs exhibit a reversed gravitational gradient in FV compared to the native lungs, a common feature of severe lung diseases in non-transplanted patients. The bilateral transplant patients reveal several different trends, potentially indicative of various stages of recovery or decline. Subject LTX5, for example, closely resembles the healthy subject with homogeneity between right and left lungs and the gravitational gradient in FV, while subject LTX3, on the other hand, exhibits opposing trends between the right and left lungs.
Conclusion
Retrospective gating of HXe images acquired during free breathing can better quantify steady-state, physiological ventilation dynamics and reveal functional differences between unilateral and bilateral transplants.Acknowledgements
No acknowledgement found.References
1. Hernandez R, et al. Lung Transplantation in Idiopathic Pulmonary Fibrosis. Medical Sciences. 2018;6:68
2. Hamedani H, et al. Quantifying Ventilation Using Dynamic Xenon MRI During Free Breathing. Proc. Intl. Soc. Mag. Reson. Med. 2022;30:3568
Figures
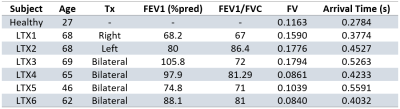
Table 1. Subject Demographics, relevant
spirometry, and mean FVs and arrival times.
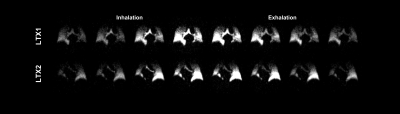
Figure 1. Representative
coronal slice of right- and left-lung unilateral transplant patients, respectively,
across the breathing cycle after registration.
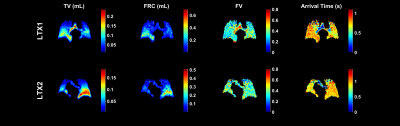
Figure 2. Maps of TV, FRC, FV,
and arrival time for a
representative coronal slice in the
right- and left-lung unilateral transplant patients, respectively.

Figure 3. Each subject’s right
and left lung averages for each map from anterior-to-posterior. Dashed lines
indicate the native lung in the case of unilateral transplant.
DOI: https://doi.org/10.58530/2023/4509