4473
Early detection of left ventricular involvement in arrhythmogenic right ventricular cardiomyopathy by Feature Tracking1Shanxi Cardiovascular Hospital, Taiyuan, China
Synopsis
Keywords: Cardiomyopathy, Quantitative Imaging
This retrospective study aimed to detect left ventricular myocardial strain by CMR-FT in ARVC patients. The 25 ARVC patients were divided into 2 subgroups: the preserved LVEF group (LVEF ≥50%, n=15) and the reduced LVEF group (LVEF <50%, n=10). The biventricular global and regional myocardial strain parameters in the radial, circumferential, and longitudinal directions were compared between ARVC and control group. ROC curve analysis showed the left ventricular basal longitudinal strain exhibited good performance in differential diagnosis between the LVEF ≥50% ARVC and the control group. In conclusion, CMR-FT can early detect left ventricular myocardial motion changes in ARVC patients.
Background
Arrhythmogenic right ventricular cardiomyopathy (ARVC) is hereditary cardiomyopathy characterized by progressive adipose or fibrous adipose tissue substitution of the right ventricular myocardium, which can also involve the left ventricle. Left ventricular involvement is not only an end-stage complication of ARVC, it can also occur in the early stage of ARVC. And left ventricular involvement is one of the risk factors for ARVC death, related to clinical arrhythmia time, heart failure severity. However, at present, the judgment of ventricular motion abnormality is mainly subjective, and objective quantitative indicators are lacking. Cardiac magnetic resonance (CMR) plays an important role in the evaluation of biventricular volumes, function, and myocardial fibrosis in patients with cardiomyopathy. In this study, the CMR-FT technique was used to analyze left ventricular myocardial strain in patients with ARVC, to objectively evaluate left ventricular motion changes, and provide an iconographical foundation for early detection of left ventricular involvementMethods
This retrospective study included patients with ARVC treated in our Hospital from October 2015 to November 2020. Healthy volunteers were enrolled as a control group. The ARVC patients were divided into 2 subgroups: the preserved left ventricular ejection fraction (LVEF) group (LVEF ≥50%) and the reduced LVEF group (LVEF <50%). All CMR cine images were imported into Canadian Circle Cardiovascular software for cardiac function and strain analysis.The software automatically plots the endocardial and epicardial boundaries and corrects them manually (Figure 1).The biventricular cardiac function parameters, global and regional myocardial strain parameters in the radial, circumferential, and longitudinal directions were compared between ARVC group, including each subgroup, and control group.Comparisons for continuous data were performed using one‐way analysis of variance.The diagnostic value of each index was evaluated by the receiver operating characteristic (ROC) curve, and the best cut-off value was selected.Results
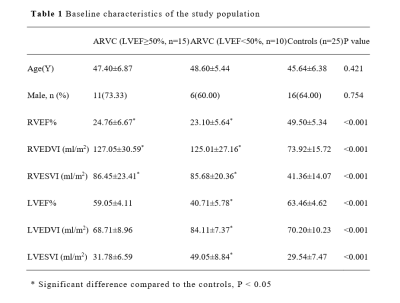
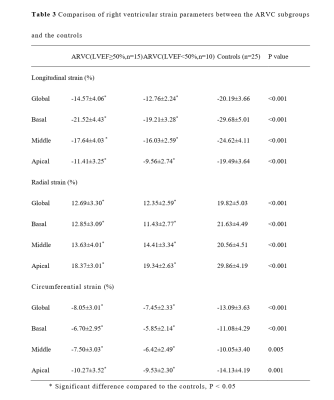
This study included 25 patients with ARVC in the ARVC group and 25 healthy volunteers in the control group. The patients with ARVC were divided into two subgroups: LVEF ≥50% (n=15) and LVEF <50% (n=10). There were no significant differences in age, sex between the ARVC group and the control group (all P>0.05). The RVEF in the two ARVC subgroups was significantly lower than that in control group, while RVEDVI and RVESVI were significantly higher than those in control group. LVEF, LVEDVI and LVESVI in the LVEF ≥ 50% ARVC group were comparable to those in the control group (all P<0.05). The LVEF in the LVEF <50% ARVC group was lower than that in the control group, while LVEDVI and LVESVI were significantly higher than those in control group (Table 1).The longitudinal, radial, and circumferential strain of the left ventricle in the LVEF <50% ARVC group were significantly lower than those in the control group (all P<0.05), while in the LVEF ≥50% ARVC group only the LV global longitudinal strain, basal and middle longitudinal strain, and basal radial strain were significantly lower than those in the control group (all P<0.05) (Table 2)Compared with the control group, the longitudinal, radial and circumferential strain of the whole right ventricle and each segment of the right ventricle in the ARVC group were significantly lower than those in the control group (all P<0.05) (Table 3).
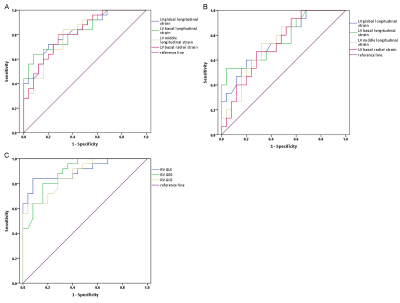
ROC curve analysis showed that compared with the other left ventricular strain parameters, the left ventricular basal longitudinal strain (AUC:0.831, 95%CI: 0.721-0.942) was better at distinguishing between ARVC patients and the control group. Moreover, the left ventricular basal longitudinal strain (AUC:0.767, 95%CI: 0.612-0.921) exhibited good performance in differential diagnosis between the LVEF ≥50% ARVC group and the control group. The AUC of right ventricular global longitudinal strain, global radial strain and global circumferential strain were 0.904, 0.893, 0.874, respectively (Figure 2).
Conclusion
CMR-FT can early detect left ventricular myocardial strain characteristic in patients with ARVC. Left ventricular basal longitudinal strain exhibited good performance in differential diagnosis.Acknowledgements
No acknowledgement found.References
1.Calkins H, Corrado D, Marcus F. Risk Stratification in Arrhythmogenic Right Ventricular Cardiomyopathy. Circulation. 2017,136:2068-2082.
2.Nagueh SF. Imaging for Risk Stratification of Sudden Cardiac Death in Patients With Arrhythmogenic Cardiomyopathy. JACC Cardiovasc Imaging. 2018,11:1387-1389.
3.Landry CH, Fatah M, Connelly KA, Angaran P, Hamilton RM, Dorian P. Evaluating the 12-Lead Electrocardiogram for Diagnosing ARVC in Young Populations: Implications for Preparticipation Screening of Athletes. CJC Open. 2021,3:498-503.
4. Aquaro GD, Pingitore A, Di Bella G et al. Prognostic Role of Cardiac Magnetic Resonance in Arrhythmogenic Right Ventricular Cardiomyopathy. Am J Cardiol. 2018,122:1745-1753.
5.Elias Neto J, Tonet J, Frank R, Fontaine G. Arrhythmogenic Right Ventricular Cardiomyopathy/Dysplasia (ARVC/D) - What We Have Learned after 40 Years of the Diagnosis of This Clinical Entity. Arq Bras Cardiol. 2019,112:91-103.
6. Paul M, Schulze-Bahr E. Arrhythmogenic right ventricular cardiomyopathy: Evolving from unique clinical features to a complex pathophysiological concept. Herz. 2020,45:243-251.
Figures
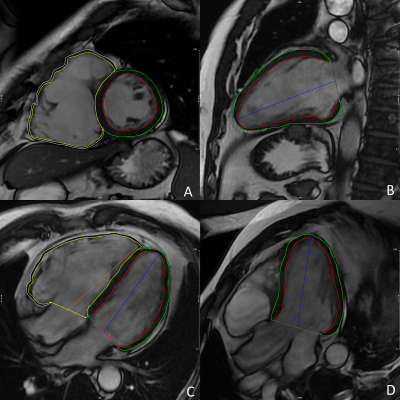
Figure 1 Myocardial strain analysis. Outlined biventricular endocardial and epicardial contours at end-diastole in the short axis (A), 2-chamber (B), 4-chamber (C), and left ventricle outflow tract (D) cine images