4466
Magnetic Resonance Imaging of Central Vein in the diagnosis of Stuck Hemodialysis Central Venous Catheter: A Case report1Guangzhou First People's Hospital, Guangzhou, China, 2Philips Healthcare, Guangzhou, China, 3Philips Healthcare, Shanghai, China, 4Philips Healthcare, Nanchang, China
Synopsis
Keywords: Vessels, Rare disease, Stuck Catheter;Central Venous;Atrial Laceration
The stuck central venous catheter (CVC) results from fibrin sheaths that firmly adhere the catheter to the wall of the superior vena cava or right atrium. Here, we report a patient with stuck CVC. The patient underwent preoperative magnetic resonance imaging (MRI) of the central vein to remove the catheter and then suffered intraoperative cardiac arrest with a bedside ultrasound suggesting cardiac tamponade and considered a right atrial laceration. The patient was then transferred to ICU, where he was discharged over a week later with stable vital signs, pending further surgery. The preoperative MRI features were analyzed retrospectively.Background
For maintenance hemodialysis patients, CVC is a common dialysis mode1. In rare cases, the fibrin sheath firmly adheres the catheter to the wall of the central vein or the right atrium, which is known as “stuck catheter” 2. However, the stuck catheter is difficult to detect preoperatively, which may lead to fatal vascular injury3,4. The MRI of the central vein could display the shape and position of the fibrin sheaths, as well as the position relationship between the fibrin sheaths, the catheter, and the vein wall. We report on a 41-year-old male with chronic kidney disease (CKD), on regular hemodialysis for 10 years and with catheter-related infection for 2 months, who had a CVC which was placed in the right internal jugular vein for more than 6 years. MRI of the central vein and digital subtraction angiography (DSA) were performed prior to the procedure to remove the catheter.MRI of central vein
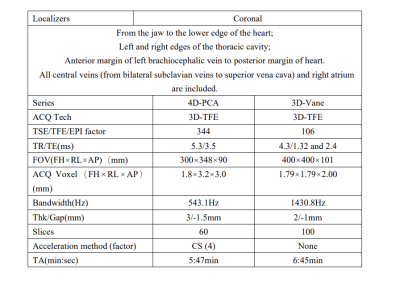
The patient was scanned on a 3.0 Tesla, Philips, Ingenia Elition X scanner, using an abdominal coil an embedded posterior coil, in a supine position. Scanning protocol included: 4D-PCA and 3D-Vane. Black blood and fat suppression for the 3D-Vane were achieved by MSDE (motion-sensitized driven-equilibrium) and mDixon. The specific parameters of the sequences are summarized in Table 1.Findings
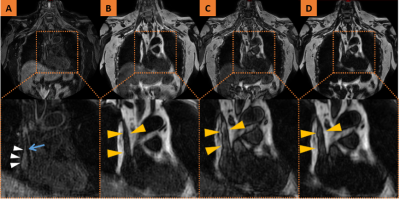
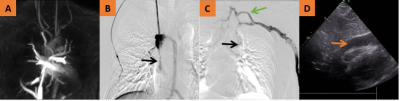
3D-Vane showed CVC indwelling from the right internal venous to the right atrium, surrounded by fibrous capsule sheath around CVC, occlusion of the superior vena cava and right brachiocephalic vein, and fibrous capsule sheath was closely related to the catheter and venous wall, and involved the right atrial wall (as seen in Fig. 1). 4D-PCA showed that the superior vena cava, bilateral brachiocephalic veins and bilateral subclavian veins were not visible, and the collateral branches of abnormal veins in the neck were open (as seen in Fig. 2A). Preoperative DSA examination and intraoperative ultrasound revealed cardiac tamponade as shown in Fig. 2B-D.Teaching Points
- The stuck CVC is usually subtle and may lead to right atrial tear and pericardial tamponade during catheter removal5.
- MRI of the central vein, as a non-contrast-enhanced, non-invasive examination, is suitable for preoperative screening.
MRI of stuck CVC
- 4D-PCA can show abnormal venous collateral opening, which is of great significance for the diagnosis of central venous stenosis or occlusion.·
- In 3D-Vane, the contour of the outer wall of the vein was shown in fat images, in-phase and out-phase images, and the luminal high-signal lesions were shown in water images. The stenosis or occlusion of the vessel could be obtained by calculation.·
- High signal lesions in 3D-Vane that contact the CVC and the central vein wall or atrial wall at the same time may be imaging signs of stuck catheter.
Conclusion
MRI of the central vein is applicable to preoperative screening and could directly observe the position and range of catheter-related fibrous capsule sheath. For patients with stuck catheter, routine catheter removal procedures may cause lacerations of the fatal right atrium.Acknowledgements
No acknowledgement found.References
1. Lok, C., T. Huber, T. Lee, S. Shenoy, A. Yevzlin, et al., KDOQI Clinical Practice Guideline for Vascular Access: 2019 Update. American journal of kidney diseases : the official journal of the National Kidney Foundation, 2020. 75: p. S1-S164.
2. Katrancioglu, N., F. Serhatlioglu, and O. Katrancioglu, An easy way to remove a stuck hemodialysis catheter. Hemodialysis international. International Symposium on Home Hemodialysis, 2021. 25(2): p. E18-E21.
3. Yongchun, H., J. Hua, H. Xiaohan, C. Jianghua, and Z. Ping, Solutions to stuck tunneled cuffed catheters in patients undergoing maintenance hemodialysis. The journal of vascular access, 2021. 22(2): p. 203-208.
4. Forneris, G., D. Savio, P. Quaretti, M. Lodi, S. Comelli, et al., Report on an Italian survey of 72 stuck hemodialysis catheters. Journal of nephrology, 2022.
5. Gameiro, J., C. Outerelo, and A. Fortes, Endovascular treatment of the stuck hemodialysis catheter: A report of two cases and literature review. The journal of vascular access, 2022: p. 11297298221074449.
Figures