4458
Preliminary Study of CMR to Evaluate Structural and Functional Alterations of the Left Ventricle in Patients with Parkinson's Disease1Radiology Department, West China Hospital, Sichuan University, Chengdu, China
Synopsis
Keywords: Cardiomyopathy, Parkinson's Disease, Cardiac magnetic resonance,Cardiac function,Myocardial strain
Parkinson's disease (PD) is the second most frequent neurodegenerative disease. Likewise, heart failure (HF) is one of the most common causes of mortality and morbidity in the world. The prevalence of HF has been found to be twice among PD patients compared with overall population regardless any other heart diseases and cardiovascular disease risk factors. Cardiac MRI is the clinically recognised gold standard for the assessment of ventricular functional parameters and myocardial histology. We have designed a study to assess the cardiac function and structure in patients with PD compared with a control group by means of cardiac magnetic resonance.Purpose
Purpose: Parkinson's disease (PD) is a chronic neurodegenerative disease commonly seen in middle-aged and older adults, and heart failure(HF) caused by cardiovascular autonomic dysfunction is a strong predictor of death in PD patients1,2,3. Currently, the causes of high prevalence of HF in PD are currently unknown,and there are limited clinically available tests to assess cardiac dysfunction4,5. The aim of this study was to investigate cardiovascular dysfunction and its associated influencing factors in patients with Parkinson's disease using cardiac magnetic resonance to assess structural and functional alterations in the heart in order to provide a reference for clinical diagnosis and management.Materials and methods
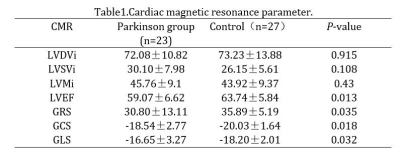
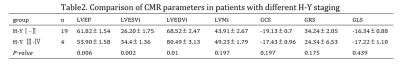
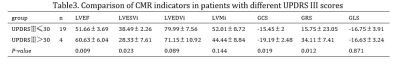
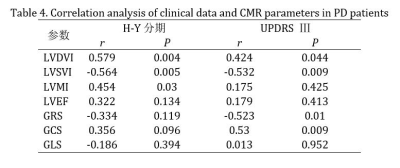
Materials and methods: 23 patients with PD (PD group) (mean age: 60 years) and 27 healthy controls (control group) (mean age: 59 years) were enrolled to undergo cardiac magnetic resonance examination, and the scanned images were analyzed for cardiac function and myocardial strain using specialized post-processing software(cvi42.5.14.2). Cardiac function parameters included left ventricular end-diastolic volume index (LVEDVi), left ventricular end-systolic volume index (LVESVi), left ventricular ejection fraction (LVEF), and left ventricular myocardial mass index (LVMi); myocardial strain parameters included left ventricular global radial strain (GRS), left ventricular global circumferential strain (GCS), and left ventricular global longitudinal strain (GLS). Patients were divided into early (H-Y stage I-II, n=15) and middle and late (H-Y stage III-IV, n=8) stages according to different disease duration [Hoehn-Yahr stage (H-Y stage)]. According to the degree of motor impairment (UPDRSⅢ), the patients were divided into UPDRSⅢ≤30 group (n=19) and UPDRSⅢ > 30 group (n=4). The differences in cardiac function and strain parameters among patients with different H-Y stages and UPDRS III scores were compared. Spearman correlation coefficient model was used to analyze the correlation between cardiac function parameters and disease severity , to explore the influencing factors of cardiac function and strain parameters.Results
Results: Analysis of cardiac function and myocardial strain showed that LVEF, GCS, GRS, and GLS were lower in the PD group than in the control group, and the differences were statistically significant (P < 0.05); the differences were not statistically significant when LVEDVi, LVESVi, GRS, GLS, and GCS were compared between groups (P > 0.05). LVEF in patients with H-Y late-stage PD was smaller than that in early stage ( 53.90±1.58 vs. 61.82±1.54,P<0.05); LVESVi, LVEDVi, and LVMi were higher in patients with late H-Y PD than in the early stage (P<0.05). LVEF, LVESVi, GCS, and GRS were lower in the UPDRS Ⅲ > 30 group than in the UPDRS Ⅲ ≤ 30 group (all P<0.05). LVEDVi, GCS, and GRS were correlated with UPDRS III scores ( all P < 0.05); LVESVi, LVEDVi, and LVMi were similarly correlated with H-Y staging in the PD group (all P < 0.05).Conclusion
Conclusion: Cardiovascular autonomic dysfunction exists in PD patients and correlates with the severity of motor symptoms. Cardiomyopathy may be one of the non-motor symptoms of Parkinson's disease.Acknowledgements
No acknowledgement found.References
1. Di Stefano C, Sobrero G, Milazzo V, et al. Cardiac organ damage in patients with Parkinson's disease and reverse dipping.[J]. Journal of hypertension, 2020,38(2):289-294.
2. Song L, Zhang S, Li H, et al. Comparison of risk factors for Parkinson's disease, coronary events and ischemic stroke.[J]. NPJ Parkinson's disease, 2022,8(1):107
3. Piqueras-Flores J, López-García A, Moreno-Reig Á, et al. Structural and functional alterations of the heart in Parkinson's disease.[J]. Neurological research, 2018,40(1):53-61.
4. El Mokadem M O, Hassan A, Hussein M, et al. The potential role of 2D-speckle tracking echocardiography for detecting left ventricular systolic dysfunction in patients with Parkinson's disease: a case control study.[J]. Acta cardiologica, 2021,76(9):979-986.
5. Alves M, Caldeira D, Ferro J M, et al. Does Parkinson's disease increase the risk of cardiovascular events? A systematic review and meta-analysis.[J]. European journal of neurology, 2020,27(2):288-296.