4435
The Effect of Breathing on Pulmonary Blood Flow using Pseudocontinuous Arterial Spin Labeling (PCASL) in a Test-Retest Design1Department of Diagnostic and Interventional Radiology, University Hospital of Tübingen, Tübingen, Germany, 2High-Field MR Center, Max Planck Institute for Biological Cybernetics, Tübingen, Germany, 3Section of Experimental Radiology, Department of Radiology, University Hospital of Tübingen, Tübingen, Germany
Synopsis
Keywords: Lung, Arterial spin labelling, Pulmonary blood flow, Lung perfusion
PCASL can quantitively measure pulmonary blood flow and detect pulmonary embolism. However, patients suffering from lung embolisms are usually unable to follow breathing commands required for optimal imaging. In this study, the influence of respiratory states on pulmonary perfusion measured with PCASL was investigated. Nineteen healthy volunteers were studied with an ECG-triggered PCASL sequence in a test-retest design. It was found that mean perfusion was highest during expiration, followed by free breathing and lowest in inspiration. A significant difference was observed between the maximal inspiration and expiration breath-hold conditions. Perfusion values acquired by PCASL in the lung parenchyma showed high reproducibility.
Introduction
Previous studies showed that pseudocontinuous arterial spin labeling (PCASL) can measure lung perfusion quantitively and detect lung embolisms1. Patients suffering from lung embolisms mostly can’t adhere to breathing commands needed for optimal imaging. The aim of this study was to detect the effects of breathing on the measured lung perfusion through PCASL.Methods
The study was approved by the local ethics committee. We examined nineteen healthy volunteers (28.0 ± 1.2 years, 14 female) using a 1.5T whole body MRI scanner (Magnetom Avantofit, Siemens Healthcare AG, Erlangen, Germany) in supine position at two separate timepoints on the same day. We measured pulmonary perfusion using an ECG-triggered PCASL sequence with fast bSSFP data acquisition. The pulmonary trunk was labeled during systole and the data was acquired in diastole of the next cardiac cycle. Labeling parameters were: duration, 400 ms; PLD, 1000 ms; flip angle, 25°. The parameters of bSSFP sequence were: TE/TR 0.9/2.1ms; flip angle, 70°; bandwidth, 1260 Hz/Px, slice thickness, 20 mm; matrix, 144×192; FoV, 480×480 mm2. We acquired perfusion data in coronal orientation in free-breathing (FB) and timed breath-hold on normal expiration (BH ModExp). Additionally, at the first timepoint we also acquired timed breath-hold on maximum inspiration (BH MaxInsp) and maximum expiration (BH MaxExp). To reduce motion artefacts imaging data were registered by the open-source toolbox elastix2,3 using an in-house developed MATLAB® (The MathWorks, Natick, MA) script. For quantitative comparison of the lung tissue perfusion measured in various breathing states, the lung parenchyma was segmented using a Gaussian mixture model4. The perfusion values of the lung were calculated as reported previously1,5. Statistical analysis was carried out using SPSS (IBM SPSS Statistics,Armonk, NY) software.Results
Results of perfusion evaluation (mean±SD) are summarized in Table 1. Mean perfusion was highest in expirations, followed by free breathing and lowest in inspiration. Kolmogorov-Smirnov test revealed normal distribution. Mauchly’s test rejected sphericity with χ2(5) = 26.58, p < .001. Friedman’s test revealed a significant effect of breathing on perfusion with χ2(3) = 29.46, p < .001. Bonferroni corrected post hoc tests showed significant difference between BH MaxInsp vs. both BH ModExp and BH MaxExp (both p < .001). For test-retest data Bland-Altman-plots revealed good comparability (Figure 1). This is supported by Friedman’s test that did not reveal significant differences. A representative example of perfusion images is depicted in Figure 2.Discussion
Under free-breathing conditions and in normal expiration, quantitative perfusion values in lung parenchyma acquired by PCASL show a high reproducibility in volunteers. Though there is an effect of the depth of breathing on perfusion the gathered data during free-breathing does not differ significantly from optimal or extreme conditions. Significant lower perfusion values/volume were found for maxInsp which needs to be investigated more in detail in the future. These results provide support for the quality of free-breathing PCASL for patients with low adherence to normal breathing.Acknowledgements
No acknowledgement found.References
1. Seith F, Pohmann R, Schwartz M, et al. Imaging Pulmonary Blood Flow Using Pseudocontinuous Arterial Spin Labeling (PCASL) With Balanced Steady-State Free-Precession (bSSFP) Readout at 1.5T. J Magn Reson Imaging. 2020;52:1767-82.
2. Klein S, Staring M, Murphy K, et al. Elastix: a toolbox for intensity based medical image registration. IEEE Trans Med Imaging 2010;29:196–205.
3. Shamonin DP, Bron EE, Lelieveldt BPF, et al. Fast Parallel Image Registration on CPU and GPU for Diagnostic Classification of Alzheimer’s Disease. Front Neuroinform 2014;7:50.
4. Walker SC, Asadi AK, Hopkins SR, et al. A statistical clustering approach to discriminating perfusion from conduit vessel signal contributions in a pulmonary ASL MR image. NMR Biomed 2015;28:1117–24.
5. Bolar DS, Levin DL, Hopkins SR, et al. Quantification of Regional Pulmonary Blood Flow Using ASL-FAIRER. Magn Reson Med 2006;55:1308–17.
Figures
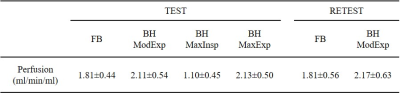
Table 1: Quantitative perfusion values (mean±SD) measured in different breathing states.
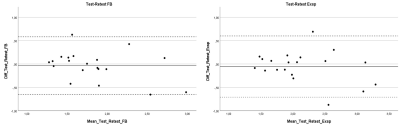
Figure 1: Bland-Altman plots for test-retest perfusion data measured in free breathing and timed breath-hold on normal expiration conditions.
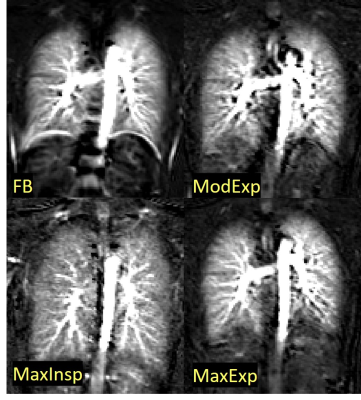
Figure 2: PCASL perfusion-weighted images of the lungs of a healthy volunteer in different respiratory states: free-breathing (FB), normal expiration (ModExp), maximum expiration (MaxExp), and maximum inspiration (MaxInsp).