4396
PET-MRI lymph node analysis, a predictive tool for recurrence in upper aerodigestive tract cancers1ICM, Paris, France, 2APHP, Pitié Salpêtrière, Paris, France
Synopsis
Keywords: PET/MR, Head & Neck/ENT, ENT, head and neck, PET/MRI, lymph nodes
The aim of our study was to analyze the imaging characteristics of lymph nodes on pre-operative PET-MRI to find the predictors of recurrence or progression.273 patients with ATD cancer who underwent PET-MRI were included. Lymph node PET/MR analysis has shown that the strongest predictors of the recurrence were lymph node enhancement and SUVmax for the controlateral nodes and enhancement, SUVmax node shape for the homolateral nodes. In conclusion, PET-MRI can be an interesting tool in the pre-therapeutic assessment of primary tumors of the ADT with lymph node extension, particularly in the identification of predictive characteristics of recurrence or progression.INTRODUCTION
Upper aerodigestive tract (ADT) cancers, mostly represented by squamous cell carcinomas (HNSCC) (90% of head and neck 1 cancers), represent the 6th most common cancer worldwide2. HNSCC have a high recurrence rate and represent one of the most common histological types to metastasize to regional lymph nodes3.Metastatic nodes are mostly homolateral to the primary tumor, but contralateral or bilateral nodes are not rare especially when the primary tumor is medial or posterior4. The risk of lymph node metastasis occurs for the largest tumors, mostly T3-T4. The presence of metastatic nodes reduces significantly the 5-year survival rate4-5.
Lymph node are accessed by CT and MRI, mostly based on size and some morphology criteria with a lack of specificity 5. 18F-FDG PET and advanced MRI methods, such as dynamic MRI and DWI, are also useful for detection of lymph node metastases6-9.
Few studies have evaluated cervical lymph nodes in ENT cancers on PET MRI. It was observed that hybrid PET-MRI imaging was both sensitive to the presence of primary tumors, as well as to cervical nodes and recurrent tumors10. PET/MRI has also been shown to be of value in post-radiation imaging 10.
While the homolateral lymph nodes are usually resected the controlateral are resected only if highly suspected to be invaded. In this context in is extremely important to detect on the baseline imaging the signes of controlateral node invasion for the correct management. Moreover no study have analyzed if semiological signs in PET-MRI can be predictors of recurrence or progression.
The aim of our study was to analyze the imaging characteristics of lymph nodes on pre-operative PET-MRI to find the predictors of recurrence or progression.
MATERIALS AND METHODS
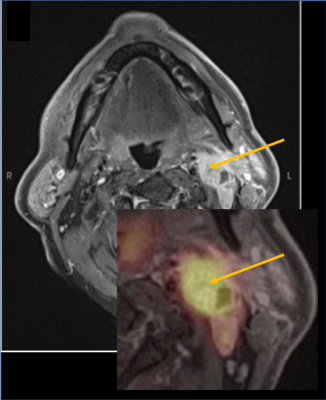
Patients : 273 consecutive patients with histo-pathologically confirmed ATD cancer who underwent PET-MRI in our institution between 2015 and 2020 were retrospectively included. For each patient, the histological type of tumor, the presence of active smoking and chronic alcoholism, and for cases of recurrence, the location of the recurrence were recorded. The patients were divided into two groups, a "case" group, subdibvised itself into two subgroups : "Recurrence," and "Progression" and a "control" group, represented by patients with primary tumor of the VATD with lymph node extension but no recurrence after management.Image acquisition: The examinations were performed on PET/MRI scanner (SIGNA 3 Tesla, GE-Healthcare, Milwaukee, USA), 60 min after injection of 3 to 5 MBq/kg of 18FDG. The MR sequences included axial T2 (IDEAL) FSE, axial T1 FSE, diffusion weighted imaging, arterial spin labelling (ASL), 3D T1 FSE after fat saturation and injection of gadoterate meglumine. The PET was performed simultaneously with a 256x256 array on the head and neck and lasted 16 minutes followed by a simultaneous whole-body PET/MRI acquisition from the neck to the proximal femurs, including four 192x192 arrays on the rest of the body, accompanied by a T1 lavaflex MRI sequence on the whole body. Image analysis: Two radiologists analyzed each lymph node aspect (signal, shape, enhancement after injection, periglionic environment, central necrosis, presence of micro or macrocalcifications, appearance of the lymph node hilum), as well as measured the size and quantitative (size), and cellularity and the vascularization represented by DWI (apparent diffusion coefficient (ADC)) and ASL analysis (cerebral blood flow). The semi-quantitative standardized uptake value (SUVmax) was measured by nuclear physicians experienced in head and neck imaging (15 years of experience). The whole was performed on an Advantage Workstation (AW4.6, GE Healthcare, Milwaukee, USA) (fig1).
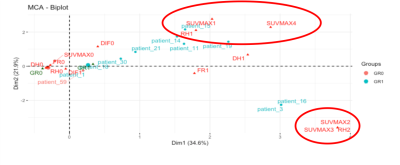
Statistical analysis: R core team 2021 software was used for performing first a multiple correspondence analysis, which allowed us to identify the underlying structure of the data, then the global and individual analysis of the variables according to the identified dimensions. A v-test was performed to compare the discriminating categorical variables.
RESULTS
For the lymph nodes controlateral (fig2) to the tumor multiple correspondence analysis revealed three dimensions that explained 71% of the total variance. In this analysis, the semiological signs. including lymph node enhancement (RH), disappearance of the ganglionic hilum (DH) and SUVmax appeared to be statistically discriminating between the "control" and "case" groups.For the lymph nodes homolateral to the tumor the parameters discriminating the "control" and "case" groups in at least one dimension included central necrosis (CN), lymph node margins (MG), blurred margins (MG2) disappearance of the hilum (DH), enhancement (HR), whether intense and homogeneous (HR1) or intense and heterogeneous (HR2) SUVmax>6 , the lymph node shape (FR), whether it is rounded (FR1) or spiculated (FR2), peri-ganglionary fat (GPG), infiltrated (GPG1). The criteria of HR, SUVMAX, and FR were the most discriminating, as they represent a high percentage in two dimensions, as shown in the overall analysis.
DISCUSSION AND CONCLUSION
While lymph node PET/MR analysis in HNSCC tumors the strongest predictors of the recurrence were lymph node enhancement (RH), disappearance of the ganglionic hilum (DH) and SUVmax for the controlateral and lymph node enhancement (RH), SUVmax and the lymph node shape for the homolateral nodes. Interestingly size, ADC or rCBF were not predictors of recurrence.In conclusion, PET-MRI can be an interesting tool in the pre-therapeutic assessment of primary tumors of the ADT with lymph node extension, particularly in the identification of predictive characteristics of recurrence or progression.
Acknowledgements
No acknowledgement found.References
1. Mody MD, Rocco JW, Yom SS, Haddad RI, Saba NF. Head and neck cancer. The Lancet. déc 2021;398(10318):2289-99.
2. Johnson DE, Burtness B, Leemans CR, Lui VWY, Bauman JE, Grandis JR. Head and neck squamous cell carcinoma. Nat Rev Dis Primer. déc 2020;6(1):92.
3. Dangore-Khasbage S. Local Metastasis in Head and Neck Cancer - an Overview. In: Marcu LG, éditeur. Contemporary Issues in Head and Neck Cancer Management [Internet]. InTech; 2015
4. Athanassios Argiris. Head and neck cancer. The Lancet. 2008;371:1695-709
5. Eisenmenger LB, Wiggins RH. Imaging of Head and Neck Lymph Nodes. Radiol Clin North Am. janv 2015;53(1):115-32.
6. Yoon DY, Hwang HS, Chang SK, Rho YS, Ahn HY, Kim JH, et al. CT, MR, US, 18F-FDG PET/CT, and their combined use for the assessment of cervical lymph node metastases in squamous cell carcinoma of the head and neck. Eur Radiol. mars 2009;19(3):634-42.
7. Heusch P, Sproll C, Buchbender C, Rieser E, Terjung J, Antke C, et al. Diagnostic accuracy of ultrasound, 18F-FDG-PET/CT, and fused 18F-FDG-PET-MR images with DWI for the detection of cervical lymph node metastases of HNSCC. Clin Oral Investig. avr 2014;18(3):969-78.
8. Varoquaux A, Rager O, Dulguerov P, Burkhardt K, Ailianou A, Becker M. Diffusion-weighted and PET/MR Imaging after Radiation Therapy for Malignant Head and Neck Tumors. RadioGraphics. sept 2015;35(5):1502-27.
9. Varoquaux A, Rager O, Lovblad KO, Masterson K, Dulguerov P, Ratib O, et al. Functional imaging of head and neck squamous cell carcinoma with diffusion- weighted MRI and FDG PET/CT: quantitative analysis of ADC and SUV. Eur J Nucl Med Mol Imaging. juin 2013;40(6):842-52.
10. Becker M, Zaidi H. Imaging in head and neck squamous cell carcinoma: the potential role of PET/MRI. Br J Radiol. avr 2014;87(1036):20130677.
Figures