4301
Application of cardiac diffusion imaging with second-order motion compensation and breath hold in the diagnosis of acute myocardial infarction1Peoples hospital of ningxia hui autonomous region, Yinchuan, China, 2Philips Healthcare, Beijing, China
Synopsis
Keywords: Heart, Cardiovascular, Heart; magnetic resonance imaging; myocardial diffusion imaging; myocardial infarction
Cardiac magnetic resonance imaging can non-invasively evaluate the anatomy and function of the heart, and has been widely used in various fields of cardiovascular diseases. This study explores the diagnostic value of DWI in the evaluation of acute myocardial infarction. The preliminary results of 17 patients showed that the ADC value of infarcted myocardium was significantly reduced, and DWI had the ability to diagnose acute myocardial infarction.Synopsis
Cardiac magnetic resonance imaging can non-invasively evaluate the anatomy and function of the heart, and has been widely used in various fields of cardiovascular diseases. This study explores the diagnostic value of DWI in the evaluation of acute myocardial infarction. The preliminary results of 17 patients showed that the ADC value of infarcted myocardium was significantly reduced, and DWI had the ability to diagnose acute myocardial infarction.Introduction
Incidence of ischemic cardiomyopathy in China is increasing year by year, which seriously endangers human health. Cardiac magnetic resonance imaging is one of the non-invasive cardiac examination methods for evaluating cardiac anatomical structure and functional parameters, which has been widely used in various fields of cardiovascular diseases and has become an important method for comprehensive and effective evaluation of ischemic cardiomyopathy. Late Gadolinium Enhancement (LGE) has become the gold standard for evaluating myocardial infarction (MI)1. However, contrast injections are contraindicated in patients with renal insufficiency, contrast allergy or other reasons. Diffusion-weighted imaging (DWI) has been widely used to diagnose acute stroke2 and has also shown good results in diagnosing ischemic or non-ischaemic heart disease3-7. However, the applicability of DWI in the evaluation of acute myocardial infarction has rarely been reported. The objective of this study is to retrospectively investigate the diagnostic performance of ADCs in the evaluation of acute myocardial infarction.Methods
Data acquisitionA total of 17 patients with suspected myocardial infarction (13 males, 4 females, mean age: 57.75 years) were included in this study, And the MRI LGE images showed delayed enhancement. All patients were scanned with a 16-channel body coil on a Philips 3T scanner (Ingenia CX, Best, Netherlands). Under ECG gating and respiratory navigation, cardiac DWI were acquired using a single EPI sequence in the short-axis view and 3 orthogonal directions. Scanning parameters: TR=3RR interval, TE=61ms; FA=90°; Voxel size = 3.5x3.5x8.0mm; Three b values were acquired within one breath hold, i.e. 0, 20, and 400 s/mm². The study was approved by the Ningxia Hui Autonomous Region People's Hospital Institutional Review Committee, and all subjects provided written informed consent.
Data analysis
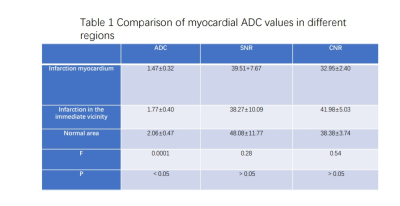
On the left ventricular short-axis image, infarct area, infarct adjacent area, and distal healthy myocardium on DWI images were drawn according to the range of delay enhancement in the LGE image (avoiding motion artifacts during delineation) to measure the average signal intensity of infarcted myocardium, adjacent myocardium, and healthy myocardial areas, respectively (SI) and standard deviation (SD), the mean signal intensity (SI) and standard deviation (SD) of the blood pool and erector spinal muscle of the same slice are measured at the same time, and the signal-to-noise ratio (SNR) and contrast noise ratio (CNR) of the image are calculated, and the SNR is calculated as: mean myocardial signal intensity (SI)/standard deviation of blood pool (SD); CNR is calculated as: (mean signal intensity of myocardium - mean signal intensity of blood pool) / standard deviation of myocardium ² + erector spinal muscle². The region of interest (ROI) is 60mm² in size, and the position and area should be as uniform as possible. All DWI images were then analyzed to obtain difusion images and measure ADC values in infarcted myocardium, adjacent myocardium, and healthy myocardial regions. (Table 1). Statistical analysis: Statistical analysis using SPSS 21.0. ADCs for 3 regions were compared using one-way ANOVA and LSD was used for comparison. P<0.05 was considered statistically significant.
Results
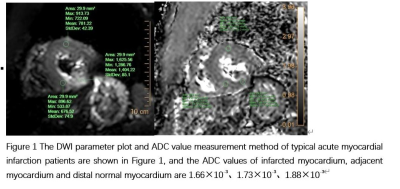
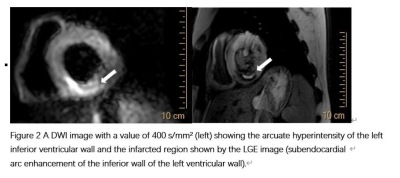
The DWI parameter plot and ADC value measurement method of typical acute myocardial infarction patients are shown in Figure 1, and the ADC values of infarcted myocardium, adjacent myocardium and distal normal myocardium are1.66×10-3、1.73×10-3、1.88×10-3. A DWI image with a value of 400 s/mm² (left) showing the arcuate hyperintensity of the left inferior ventricular wall and the infarcted region shown by the LGE image (subendocardial arc enhancement of the inferior wall of the left ventricular wall). The ADC values of infarcted myocardium, myocardium adjacent to infarction and distal normal myocardium were calculated as 1.47±0.32, 1.77±0.40, 2.06±0.47, P<0.05, respectively, the difference was statistically significant, and the ADC value of infarcted myocardium was the lowest, which was significantly lower than that of myocardium adjacent to infarction and distal normal myocardium. However, there was no significant difference in CNR and SNR between infarcted myocardium and myocardium adjacent to infarction and distant healthy myocardium (P>0.05).Discussion and conclusion
This study showed that the ADC values of infarcted myocardium, myocardial adjacent to infarction and healthy myocardial region obtained by myocardial diffusion imaging (DWI) in breath-hold mode were significantly different, showing good diagnostic value for infarcted myocardium. This may be due to the fact that the early stage of acute myocardial infarction is mainly manifested as cytotoxic edema in cardiomyocytes, the extracellular space is reduced, and the movement of water molecules is restricted, while DWI can reflect the restricted diffusion of water molecules in tissues and lesions, so as to manifest as a decrease in ADC value in acute infarction myocardium, and DWI is hyperintensive.Acknowledgements
No Acknowledgements foundReferences
1.Pattanayak P, Bleumke DA. Tissue characterization of the myocardium: state of the art characterization by magnetic resonance and computed tomography imaging. Radiol Clin North Am. 2015;53(2):413-423. doi:10.1016/j.rcl.2014.11.005
2.Lovblad KO, Laubach HJ, Baird AE, Curtin F, Schlaug G, Edelman RR, Warach S. Clinical experience with di usion-weighted MR in patients with acute stroke. AJNR Am JNeuroradiol 1998;19(6):1061-1066.
3.Deux JF, Maatouk M, Vignaud A, Luciani A, Lenczner G, Mayer J, Lim P, Dubois-Rande JL, Kobeiter H, Rahmouni A. Di usion-weighted echo planar imaging in patients withrecent myocardial infarction. Eur Radiol 2011;21(1):46-53.
4.Laissy JP, Gaxotte V, Ironde-Laissy E, Klein I, Ribet A, Bendriss A, Chillon S, Schouman-Claeys E, Steg PG, Serfaty JM. Cardiac di usion-weighted MR imaging in recent,subacute, and chronic myocardial infarction: a pilot study. J Magn Reson Imaging 2013;38(6):1377-1387.
5.Xiang SF, Zhang XQ, Yang SJ, Gao YY, Gao BL, Shi QL, Li S. Intravoxel Incoherent Motion Magnetic Resonance Imaging with Integrated Slice-speci c Shimming for oldmyocardial infarction: A Pilot Study. Sci Rep 2019;9(1):19766.