4279
Comparison of integrated slice-specific dynamic shimming and echo-planar imaging diffusion-weighted imaging in bladder cancer detection and characterization
yujiao zhao1, cong you1, cheng zhang1, feifei qu2, jinxia zhu2, and Thomas Benkert3
1The First Central Clinical College of Tianjin Medical University, tianjin, China, 2MR collaborations, Siemens Healthcare, beijing, China, 3MR Application Predevelopment, Siemens Healthcare GmbH, Erlangen, Germany
1The First Central Clinical College of Tianjin Medical University, tianjin, China, 2MR collaborations, Siemens Healthcare, beijing, China, 3MR Application Predevelopment, Siemens Healthcare GmbH, Erlangen, Germany
Synopsis
Keywords: Urogenital, Bladder, bladder cancer
This study investigated the image quality and lesion characterization of bladder lesions on integrated slice-specific dynamic shimming (iShim) diffusion-weighted imaging (DWI) compared with single-shot echo-planar imaging (ss-EPI) DWI. The qualitative and quantitative image quality analyses were compared between the 2 DWI techniques. The diagnostic agreements of lesion characterization, including submucosal stalk and myometrial invasion, were also evaluated on DWI images compared with pathologic results. The results indicated that iShim-DWI provided better bladder tumor detection and image quality than ss-EPI DWI, suggesting that iShim-DWI might serve as a competent technique in bladder imaging.Abstract
Introduction and Purpose:Diffusion-weighted imaging (DWI) has been routinely used as the clinical sequence in pelvic imaging. However, single-shot echo-planar imaging (SS-EPI) DWI was challenging in bladder lesion detection and evaluation due to limited spatial resolution, sensitivity to motion, and magnetic susceptibility artifact [1-2].
Integrated slice-specific dynamic shim (iShim) DWI with post-processing distortion correction to conventional 3D volume shim reduces artifacts and signal loss [3]. Recently, iShim-DWI has been reported to improve image quality and lesion detection in the prostate, breast, and thyroid [4–6].
This study aimed to compare the bladder imaging quality and discriminational ability of lesion characterization between iShim-DWI and ss-EPI DWI.
Materials and Methods: This study prospectively enrolled 45 consecutive patients with bladder cancer having 46 lesions. All the patients underwent iShim-DWI performed by a prototype sequence
and ss-EPI-DWI before the surgery on a 3T system (MAGNETOM Prisma, Siemens Healthcare, Erlangen, Germany). The parameters were as follows: ss-EPI-DWI, TR = 3300 milliseconds, TE = 49 milliseconds, slice thickness = 3 mm, slice gap = 0.3 mm, NEX = 12, FOV = 300 × 300 mm2, matrix = 128 × 128, b value = 0 and 1000 s/mm2, and scan time = 2 minutes 27 seconds; iShim-DWI, TR 2300 = milliseconds, TE = 56 milliseconds, slice thickness = 3 mm, slice gap = 0.3 mm, NEX = 12, FOV = 300 × 300 mm2, matrix = 230 × 230, b value = 0 and 1000 s/mm2, scan time = 1 minute 50 seconds. Two independent readers evaluated the qualitative analysis, including adequate fat suppression, presence of artifacts, and image quality on DWI with a high b value. The quantitative analysis was performed by measuring the standard deviation (SD) of the gluteus maximus and signal intensity of the lesion and normal bladder wall (Fig. 1) and calculating image quality parameters, such as signal-to-noise ratio (SNR)- SIlesion/SD, contrast-to-noise ratio (CNR) of the bladder lesion-(SIlesion-SIbladder wall)/SD, and signal intensity of lesion to bladder wall ratio (SIR) -SIlesion /SIbladder wall. The lesion characterizations included submucosal stalk and myometrial invasion infiltration, which was confirmed by surgical pathology and cystoscopy.
Statistical analyses were performed with SPSS software version 23.0 (IBM Corporation, Armonk, NY, USA). Bland–Altman plots were used for interobserver agreement. The qualitative and quantitative data from two DWI techniques were compared using the Wilcoxon test or paired-samples t test. Cohen's kappa was used to evaluate the diagnostic agreement of lesion characterizations on DWI techniques compared with pathologic and cystoscopic findings.
Results: We detected good interobserver reliability (Table 1). Compared with ss-EPI-DWI, iShim-DWI images indicated significantly higher scores for image quality and fat suppression (all P< 0.001). Meanwhile, iShim-DWI indicated a lower score for artifacts than SS-EPI-DWI (P < 0.001) (Table 2). Both SNR and CNR of b = 1000 s/mm2 images on iShim-DWI were higher than those of ss-EPI-DWI(Fig.1). SIR revealed no significant difference between the 2 DWI sequences (Table 3).
The kappa value of iShim-DWI in distinguishing submucosal stalk and myometrial invasion was 0.864 and 0.652, respectively, indicating a good agreement compared with pathologic results (P < 0.05) (Table 4). Meanwhile, the diagnostic agreement of the submucosal stalk and myometrial invasion on ss-EPI-DWI images was poor to moderate (k = 0.624 and 0.435, P < 0.05) (Table 4).
Discussion:
DWI helps identify the presence of bladder tumors in clinical practice. Poor spatial resolution and geometric distortion regarding magnetic field inhomogeneity caused inaccuracy in detecting and assessing bladder lesions on the ss-EPI DWI sequence in our study. iShim-DWI provided better detection and image quality in bladder imaging than ss-EPI DWI. Therefore, iShim-DWI is recommended because of its conspicuity in bladder tumor detection and image quality.
Conclusion: iShim-DWI is a promising technique with good image quality in bladder imaging and has the ability to identify bladder tumors and provide pathologic characterization.
Keywords: Bladder cancer; diffusion-weighted imaging; imaging quality; integrated slice-specific dynamic shimming; tumor characterization
Acknowledgements
NoneReferences
1. Partridge SC, Nissan N, Rahbar H, Kitsch AE, Sigmund EE. Diffusion-weighted breast MRI: clinical applications and emerging techniques. J Magn Reson Imaging. 2017;45(2):337-55.2. Jezzard P, Balaban RS. Correction for geometric distortion in echo planar images from B0 field variations. Magn Reson Med. 1995;34(1):65-73.
3. McElroy S, Winfield JM, Westerland O, et al. Integrated slice-specific dynamic shimming for whole-body diffusion-weighted MR imaging at 1.5 T. MAGMA. 2021;34(4):513-521.
4. Liney GP, Holloway L, Al Harthi TM, Sidhom M, Moses D, Juresic E, et al. Quantitative evaluation of diffusion-weighted imaging techniques for the purposes of radiotherapy planning in the prostate. Brit J Radiol. 2015; 88(1049):20150034.
5. Chen L, Sun P, Hao Q, Yin W, Xu B, Ma C, et al. Diffusion-weighted MRI in the evaluation of the thyroid nodule: Comparison between integrated shimming EPI and conventional 3D-shimming EPI techniques. Oncotarget. 2018;9(40):26209-16.
6. Lee SK, Tan ET, Govenkar A, Hancu I. Dynamic slice-dependent shim and center frequency update in 3 T breast diffusion weighted imaging. Magn Reson Med. 2014;71(5):1813–8.
Figures
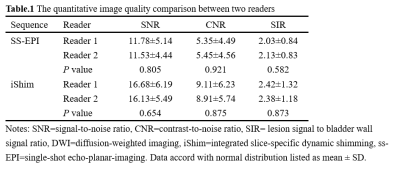
Notes: CNR, contrast-to-noise
ratio; DWI, diffusion-weighted imaging; iShim, integrated slice-specific
dynamic shimming; SIR, lesion signal to bladder wall signal ratio; SNR,
signal-to-noise ratio; ss-EPI, single-shot echo-planar-imaging. Data with normal distribution are expressed as
mean ± SD.
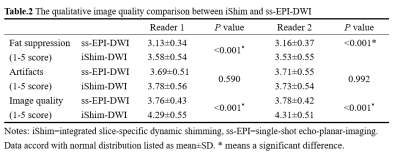
Notes: iShim,
integrated slice-specific dynamic shimming; ss-EPI, single-shot echo-planar
imaging. Data with normal
distribution are expressed as mean ± SD. * means
a significant difference. DWI, diffusion-weighted
imaging; iShim, integrated slice-specific dynamic shimming; ss-EPI, single-shot
echo-planar-imaging
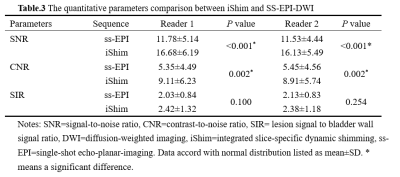
Notes: CNR, contrast-to-noise ratio; DWI, diffusion-weighted imaging; iShim, integrated slice-specific dynamic shimming; SIR, lesion signal to bladder wall signal ratio; SNR, signal-to-noise ratio; ss-EPI, single-shot echo-planar-imaging. Data with normal distribution are expressed as mean ± SD. * means a significant difference.
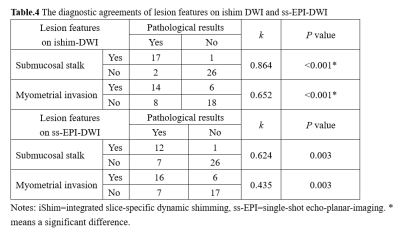
Notes: iShim,
integrated slice-specific dynamic shimming; ss-EPI, single-shot echo-planar
imaging. * means a
significant difference.
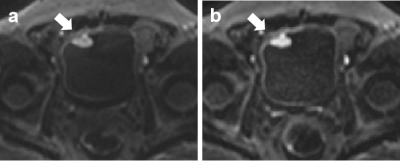
Fig.1 Comparison
between iShim- and ss-EPI-DWI in patients with bladder cancer(arrow). ss-EPI-DWI(a)
showed higher SNR and CNR with lower signal noise compared with iShim-DWI(b).
DOI: https://doi.org/10.58530/2023/4279