4275
Readout-segmented echo-planar imaging in the evaluation of anal fistula: Comparison with single-shot echo-planar diffusion-weighted imaging1Radiology Department, The Affiliated Hospital of Southwest Medical University, LuZhou, China, 2Radiology Department, The affiliated Hospital of Southwest Medical University, LuZhou, China, 3SIEMENS Healthineers Ltd.Shanghai, Shanghai, China
Synopsis
Keywords: Pelvis, Diffusion/other diffusion imaging techniques
To assess the image quality of anal fistula by RESOLVE DWI compared to SS-EPI DWI, and explore the value of RESOLVE DWI for diagnosis and classification of anal fistula. Qualitative and quantitative evaluation of image quality showed that RESOLVE DWI group was superior than SS-EPI DWI group.The accuracy of RESOLVE DWI sequence in the diagnosis of the internal orifice, branch fistula, and classification was higher than in SS-EPI DWI for anal fistula. RESOLVE DWI can provide higher quality images of anal fistula than SS-EPI DWI.Introduction/Purpose
Recent studies have shown that DWI combined with fat-suppressed T2-weighted imaging could increase the conspicuity of anal fistulae (1-5). However, the traditional DWI based on single-shot echo-planar imaging (SS-EPI) is prone to image artifacts like geometric distortions, image blurring, and ghosting artifacts (6). RESOLVE DWI is a novel type of DWI scanning sequence, which can reduce the accumulation of phase errors in the phase coding direction and shorten the sampling time, generating high-resolution DWI images (7). Several studies have applied RESOLVE DWI to examine pelvic lesions such as rectal cancer, prostate cancer, and cervical cancer, suggesting that this sequence could generate high-quality images (6.8-10). Yet, the use of RESOLVE DWI on evaluating anal fistula has not been reported.The aim of this study was to compare the sensitivity and specificity of RESOLVE DWI and SS-EPI DWI when assessing anal fistula. In addition, we evaluated the value of RESOLVE DWI in the preoperative diagnosis of an anal fistula to obtain the best DWI sequence and provide a reference for the imaging diagnosis of anal fistula in the future.Method
A total of 34 patients suspected of an anal fistula were included in the study. Imaging was performed with a 3.0-T MRI scanner (Magnetom Prisma, Siemens Healthcare, Erlangen, Germany) with 18-channel phased-array body coil. The detailed SS-EPI DWI and RESOLVE DWI sequence parameters are summarized in Table 1.The axial and coronal scans were planned perpendicular and parallel to the long axis of the anal canal, respectively. All patients underwent RESOLVE DWI and SS-EPI scanning of the anal canal oblique cross-section. Images reconstruction of diffusion sensitive gradient b value 50 s/mm2 and 800 s/mm2 was completed. All the measurements and evaluations were conducted by Siemens 3.0 T Skyra MR work station (version Syngo MR D13). MR images were analyzed (b 800s/mm2) based on four aspects: lesion conspicuity, anatomical details, geometric distortion and ghosting artifacts, and overall image quality.Paired Wilcoxon’s signed-rank tests were used to assess the qualitative score of image quality. Paired t-test was used to compare the differences in SNR and CNR between RESOLVE DWI and SS-EPI DWI images at the same b-value. The accuracy of an internal orifice, branch fistula, and preoperative classification of anal fistula by RESOLVE DWI and SS-EPI DWI were calculated according to surgical results. The difference between the RESOLVE DWI and SS-EPI DWI group was tested by Fisher's exact probability method. Differences among the data were considered statistically significant at a P-value < 0.05.Result
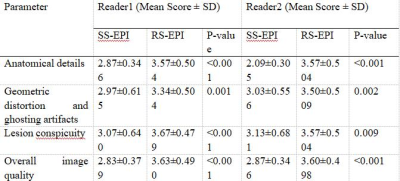
The anatomical details, geometric deformation and artifacts, lesion significance, and overall image quality score of the RESOLVE DWI sequence were higher than those of the SS-EPI sequence (all P < 0.05) (Table 2). Examples of RESOLVE DWI's advantages are shown in Figure 1 and 2.The average values of SNR for SS-EPI DWI and RESOLVE DWI were 313.61 ± 114.84 and 130.29 ± 51.10, respectively (P<0.001, 95% CI: 146.53–220.09). On the other hand, the average values of CNR were higher for SS-EPI (219.22 ± 102.77) than those for RESOLVE DWI (102.42 ± 47.47)(P < 0.001, 95% CI: 89.08–144.53). Compared with the surgical results, the accuracy of SS-EPI sequence in the diagnosis of the internal orifice, primary fistula, branch fistula, and the abscess was 84.85% (28/33), 100% (30/30), 76.47% (13/17), and 100% (18/18), respectively, while the accuracy of RESOLVE DWI sequence in the internal diagnosis orifice, primary fistula, branch fistula, and the abscess was 93.94% (31/33), 100% (30/30), 94.12% (16/17), and 100%(18/18), respectively; there was no significant difference in the accuracy of SS-EPI and RESOLVE DWI sequences (P>0.05). Moreover, according to Morris's classification, the accuracy of SS-EPI and RESOLVE DWI in the classification of the anal fistula was 86.67% (26/30) and 93.33% (28/30), respectively; the results showed no significant difference in the accuracy of classification between the two methods (P>0.05).Discussion
RESOLVE is a new RS-EPI technology that relies on 2D navigation technology. It could turn the K-space acquisition tracks into multiple connecting channels and continuously collect images, thus shortening the readout time of gradient pulses and improving image fidelity (11). Our research showed that RESOLVE DWI was superior to SS-EPI DWI sequence in assessing anatomical details, geometric deformation and artifacts, lesion significance, and overall image quality, which is consistent with the previously reported results of RESOLVE DWI in cervical cancer, prostate, rectal cancer and so on (6.8-10). In addition, the RESOLVE DWI sequence showed clearer DWI images, high spatial resolution, and slight deformation, which is helpful to distinguish small lesions and observe details of lesions.Furthermore, we found that SNR and CNR of SS-EPI DWI were higher than those of RESOLVE DWI, and the difference was statistically significant, which is consistent with the results of previous studies on prostate (12), pediatric brain (13), and breast (14).Conclusion
The application of RESOLVE DWI in the diagnosis of anal fistula could reduce magnetic sensitive artifacts and image distortion and improve image quality. It could also be used to observe more small and potential internal orifices and branches. RESOLVE DWI provides more comprehensive anatomical and pathological information for surgical treatment of anal fistula and is of great value for clinical selection of correct treatment.Acknowledgements
We acknowledge all the co-authors for their hard work in this study.References
1.Hori M; Oto A; Orrin S; et al.Diffusion-weighted MRI: a new tool for the diagnosis of fistula in ano. Journal of magnetic resonance imaging: JMRI 2009;30:1021-6.
2.Yoshizako T; Wada A; Takahara T; et al. Diffusion-weighted MRI for evaluating perianal fistula activity: feasibility study. European journal of radiology 2012; 81:2049–53.
3. Dohan A; Eveno C; Oprea R; et al. Diffusion-weighted MR imaging for the diagnosis of abscess complicating fistula-in-ano: preliminary experience. Eur Radiol 2014;24:2906-15.
4. Dohan A; Taylor S; Hoeffel C; et al. Diffusion-weighted MRI in Crohn’s disease: Current status and recommendations. Journal of magnetic resonance imaging: JMRI 2016;44:1381-1396.
5. Bakan S; Olgun DC; Kandemirli SG; et al. Perianal Fistula With and Without Abscess: Assessment of Fistula Activity Using Diffusion-Weighted Magnetic Resonance Imaging. Iranian Journal of Radiology 2015;12: e29084.
6.Qian Weiliang;Chen Qian;Zhang Zhongshuai,et al. Comparison between readout-segmented and single-shot echo-planar imaging in the evaluation of cervical cancer staging. BRITISH JOURNAL OF RADIOLOGY 2019;92: 20180293.
7. Wisner, DJ; Rogers, N; Deshpande, VS; et al. High-resolution diffusion-weighted imaging for the separation of benign from malignant BI-RADS 4/5 lesions found on breast MRI at 3T.J Magn Reson Imaging 2014;40:674-81.
8.Li, L; Wang, L; Deng, M; et al. Feasibility Study of 3-T DWI of the Prostate: Readout-Segmented Versus Single-Shot Echo-Planar Imaging. AJR Am J Roentgenol 2015; 205:70-6.
9. Xia, CC; Liu, X; Peng, WL; et al.Readout-segmented echo-planar imaging improves the image quality of diffusion-weighted MR imaging in rectal cancer: Comparison with single-shot echo-planar diffusion-weighted sequences.Eur J Radiol 2016; 85:1818-1823.
10. Xie, M; Ren, Z; Bian, D; et al. High resolution diffusion-weighted imaging with readout segmentation of long variable echo-trains for determining myometrial invasion in endometrial carcinoma.Cancer Imaging 2020; 20:66.
11. Wan, H; Sha, Y; Zhang, F; et al. Diffusion-weighted imaging using readout-segmented echo-planar imaging, parallel imaging, and two-dimensional navigator-based reacquisition in detecting acute optic neuritis.J Magn Reson Imaging 2016;43:655-60.
12. Fedorov, A; Tuncali, K; Panych, LP; et al.Segmented diffusion-weighted imaging of the prostate: Application to transperineal in-bore 3T MR image-guided targeted biopsy.Magn Reson Imaging 2016; 34:1146-54.
13. Yeom, KW; Holdsworth, SJ; Van, AT; et al.Comparison of readout-segmented echo-planar imaging (EPI) and single-shot EPI in clinical application of diffusion-weighted imaging of the pediatric brain.AJR Am J Roentgenol 2013;200:W437-43.
14. W. Bogner, K; Pinker-Domenig; H. Bickel; et al. Readout-segmented echo-planar imaging improves the diagnostic performance of diffusion-weighted MR breast examinations at 3.0 T. Radiology 2012; 263:64-76.
Figures
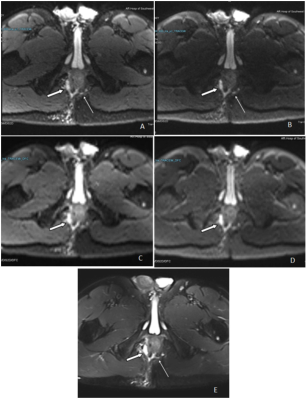
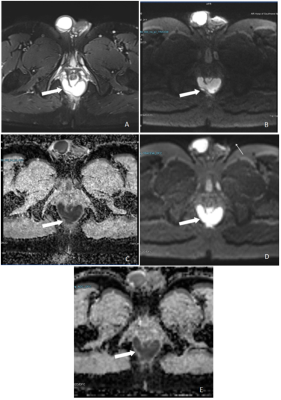
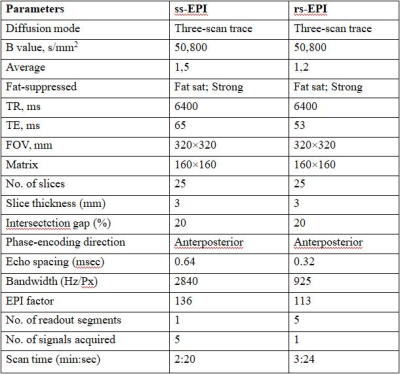
Table 1. Imaging Parameters for ss-EPI and rs-EPI DWI
Note: ssEPI, Single-Shot Echo-planar Imaging; rs-EPI, Readout-segmented Echoplanar Imaging; DWI, diffusion-weighted imaging; TR, time of repeat; TE, time of echo; FOV field of Vision