4271
MRI-based scoring model to predict massive hemorrhage during dilatation and curettage in patients with cesarean scar pregnancy1Radiology, Chengdu Women's and Children's Central Hospital, School of Medicine, University of Electronic Science and Technology of China, Chengdu, China, 2Gynecology, Chengdu Women's and Children's Central Hospital, School of Medicine, University of Electronic Science and Technology of China, Chengdu, China
Synopsis
Keywords: Urogenital, Urogenital, Cesarean scar pregnancy; Magnetic resonance imaging (MRI); Curettage; Massive hemorrhage; Risk factors
Cesarean scar pregnancy is a special type of ectopic pregnancy for which dilatation and curettage (D&C) is one of the main treatment modalities, and uncontrollable hemorrhage is a more dangerous complication during D&C. Accurate preoperative prediction of the risk of intraoperative hemorrhage will help gynecologists draw up precise treatment. The aim of this study is to develop an MRI scoring model for predicting intraoperative hemorrhage during D&C. The study found that cesarean section diverticulum area, uterine scar thickness and gestational sac diameter were independent risk factors for intraoperative hemorrhage. A scoring model was developed, The model possessed decent prediction performance.Introduction
Cesarean scar pregnancy (CSP), a special type of ectopic pregnancy where the gestational sac is implanted in the scar of the previous cesarean section, is one of the long-term complications of cesarean section. Termination of pregnancy was the principal management of CSP[1]. Dilatation and curettage (D&C) has become the mostly commonly used operation to terminate pregnancy given that it is relatively simple and easy to operate. The risk of complications during D&C varied among CSP patients with different conditions. Low-risk CSP patients could achieve minimal bleeding and complete removal of pregnancy tissue with D&C alone[2], but blind D&C without adequate preparation might lead to serious complications and even endanger the lives of the high-risk CSP patients. Medical imaging has always played an important role in the diagnosis and preoperative evaluation of CSP. MRI has been more frenquently used in the assessment of CSP patients. MRI, with multi-directional and multi-parameter imaging, could provide more information on the gestational sac and uterus, and had higher soft tissue resolution and spatial resolution[3,4]. The current application of MRI in CSP mainly focused on disease diagnosis while few of the studies[5,6]have been conducted to explore the value of MRI in massive hemorrhage prediction during D&C. Of note, these previous studies[5,6] failed to comprehensively analyze the predictive power of multi MRI signs for massive hemorrhage. The aim of this study was to construct an MRI-based quantitative scoring model to preoperatively predict the risk of massive hemorrhage during D&C in CSP.Method
Between October 2020 to July 2022, 187 CSP patients retrospectively reviewed for this study. The included patients would be randomly divided into training and validation cohort with a ratio of 7:3. MRI scans were performed using a 3.0-T unit (MAGNETOM VIDA, Siemens Healthcare, Erlangen, Germany) with an 18-channel body phased-array surface coil. The sagittal T2-weighted image of the CSP patients were obtained using spin echo sequences to assess the morphological signs of the uterus and gestational sac. Sagittal dynamic contrast-enhanced T1-weighted imaging using gradient echo sequences with fat saturation was acquired to observe the enhancement mode of uterus and gestational sac. The following MRI signs would be review by radiologists: uterine scar thickness, gestational sac growth direction, cesarean section diverticulum (CSD) depth, The position relationship between gestational sac and CSD, the marked enhancement of trophoblastic tissue in the arterial phase, area of CSD, gestational sac diameter. Univariate analysis and multivariate logistic regression analysis were used to identify the independent risk factors regarding MRI signs for massive hemorrhage. The odds ratio of each independent risk factors was used to form the risk scoring model. The Youden’s index generating from receiver operating characteristic curve (ROC) were used to obtain the optimal cut-off values for the quantitative MRI parameters and scoring models. All analyses were performed using SPSS 22.0 and MedCalc 20.0.14. A two-tailed P<0.05 is recognized as statistically significant.Results
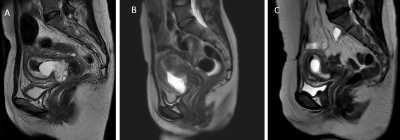
The detailed screening process was presented in Figure 1. Univariate analysis showed that all seven MRI findings were significantly associated with massive hemorrhage, and multivariate logistic regression analysis incorporating above the seven MRI signs further identified three independent risk factors (uterine scar thickness, gestational sac diameter and CSD area) (Table 1). The cutoff values for these 3 independent risk factors were 2.25 mm, 44.75 mm and 163.50 mm2, respectively. The three independent risk factors were used to construct the scoring model, where the odds ratio of each independent risk factors would be converted to the corresponding point. 8 points was identified as the optimal cutoff value to divide the patients into low-risk and high-risk groups. The ROC curves were plotted to visualize predictive power of the scoring model both in the training and validation cohort (Figure 2). The scoring model has high sensitivity, specificity, accuracy, negative predictive value, and acceptable positive predictive value in both training cohort and validation cohort (Table 2). The preoperative MRI of some subjects is shown in Figure 3.Discussion
To our knowledge, this was the first time ever to comprehensively analyze the MRI signs related to intraoperative hemorrhage and a risk scoring model was constructed accordingly in order to quantify the weight of each independent risk factors in adding to the prediction power of the model. Three independent risk factors including the area of CSD, uterine scar thickness, and gestational sac diameter for intraoperative hemorrhage were identified to develop this risk scoring model for predicting the massive hemorrhage. Notably, the three indicators incorporated into the prediction model were readily available by simple MRI plain scan, which will further expand the clinical application of the model clinically. As a result, a low risk of massive hemorrhage during D&C was indicated when the MRI-based score was less than 8 points and the pregnancy could be terminated safely and effectively through simple D&C while extra preoperative preparation including uterine artery embolization, operation mode shifting or patients transferring should be made if the score was equal to or greater than 8 points.Conclusion
Preoperative MRI examination was of great significance for the risk assessment of massive hemorrhage during D&C in CSP patients. Future prospective studies with large samples from multiple centers are needed to confirm the findings.Acknowledgements
No acknowledgement found.References
[1] Family Planning Subgroup, Chinese Society of Obstetrics and Gynecology, Chinese Medical Association. Expert opinion of diagnosis and treatment of cesarean scar pregnancy (2016) [J]. Zhonghua Fu Chan Ke Za Zhi, 2016,51(8): 568-572.
[2] Le A, Li M, Xu Y, et al. Different Surgical Approaches to 313 Cesarean Scar Pregnancies [J]. J Minim Invasive Gynecol, 2019,26(1): 148-152.
[3] Liu D, Yang M, Wu Q. Application of ultrasonography in the diagnosis and treatment of cesarean scar pregnancy [J]. Clin Chim Acta, 2018,486: 291-297.
[4] Peng KW, Lei Z, Xiao TH, et al. First trimester caesarean scar ectopic pregnancy evaluation using MRI [J]. Clin Radiol, 2014,69(2): 123-129.
[5] Du Q, Liu G, Zhao W. A novel method for typing of cesarean scar pregnancy based on size of cesarean scar diverticulum and its significance in clinical decision-making [J]. J Obstet Gynaecol Res, 2020,46(5): 707-714.
[6] Du Q, Zhao W. Exploring the value of cesarean section diverticulum area to predict the safety of hysteroscopic management for cesarean scar pregnancy patients [J]. Int J Gynaecol Obstet, 2022,156(3): 488-493.
Figures
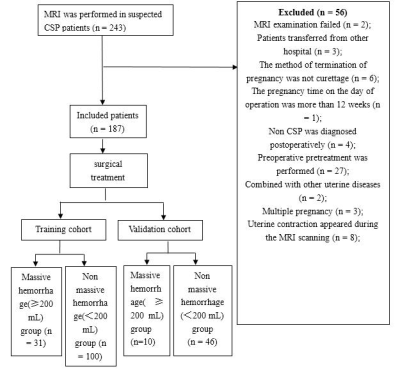
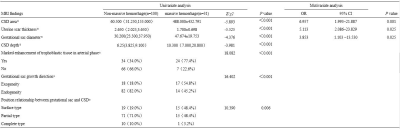
Table. 1 Univariate and multivariate logistic regression analysis on MRI findings for the prediction of intraoperative massive hemorrhage in training cohort
Data was presented as mean ± standard deviation, median (25%, 75%) and number (percent %)
CSD cesarean section diverticulum;
OR Odds Ratio;
95% CI, 95% confidence interval
a Mann-Whitney U test
b Pearson χ2 test
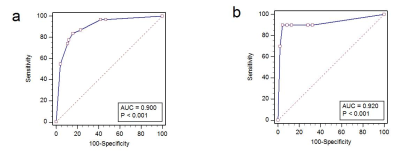

Table. 2 The predictive powers of the MRI scoring model in the training cohort and validation cohort.
AUC, area under curve;
95% CI, 95% confidence interval