4270
Magnetic Resonance Lymphangiography Manifestations and Applications in Secondary Lymphoedema1Department of Radiology, Taizhou Hospital of Zhejiang Province affiliated to Wenzhou Medical University, Taizhou, China, 2Department of Hand and Foot Surgery, Taizhou Hospital of Zhejiang Province affiliated to Wenzhou Medical University, Taizhou, China, 3Central Research Institute, United Imaging Healthcare, Shanghai, China
Synopsis
Keywords: Screening, Visualization, Lymphoedema Imaging
Surgical intervention should be considered when extremity lymphedema reached clinical stage II, and the identification of lymphatic vessels from nearby veins is critical for surgery planning. In this study, we reviewed the MRL examinations of patients with secondary lymphedema. The results showed that MRL could be used to characterize the secondary lymphedema pre-operatively, and predefine treatment planning for patients who suffer secondary lymphedema.Introduction
Lymphoedema is localised swelling of the soft tissues due to the accumulation of protein-rich fluid in the interstitial space1. While it is a progressive, chronic swelling process that can occur in any part of the body, extremities are the most affected areas1. Lymphoedema has been broadly divided into two categories: primary and secondary diseases. Secondary lymphedema can develop on people at any age since it is commonly caused by infection, malignant lymph node dissection, radiation therapy, or lymph node damage after trauma2. Previous imaging methods of lymphatics were limited to poor image qualities, while magnetic resonance lymphangiography (MRL) was proposed as a non-invasive, high-resolution, and radiation-free technique for the evaluation of lymphatic system diseases3. This study aims to explore the clinical utility of MRL in secondary lymphedema which has been sparsely investigated. We analysed the clinical stage, lymphoedema classifications, and how they were correlated with MRL findings.Methods
A total of 38 patients including 77 limbs were scanned on a 1.436T MR system (uMR 586, United Imaging Healthcare, Shanghai, China). Two sequences were adapted for the MRL imaging: a) fat-suppressed 3D turbo spin echo (3D-TSE) T2WI. b) Dynamic T1-weighted 3D gradient-recalled echo (3D T1W GRE) sequence. 3D-TSE T2WI was designed to rate the severity of oedema, and maximum intensity projection (MIP) images were reconstructed based on 3D T1W GRE sequence. Imaging parameters were listed in Table 1.Severity ratings of lymphoedema were performed by a surgeon with more than 10 years of experience according to the 2020 International Society of Lymphology guidelines. This study included patients with stage I-III lymphoedema.
MR images were independently analyzed by two radiologists. Lymphatic vessels were distinguished from veins based on the morphology and signal intensity on MIP images. Secondary lymphangiectasis was classified into two categories: lymphatic obstruction and increased lymphatic vessel patency.
Results
There were 31 patients with lymphatic vessel blockage, accounting for 81.5% of the study population. 7 of them were of stage I, 15 of stage II, and 9 of stage III. Lymphatic vessels of them were found bead-like, dilated, and had segmental occlusions, while the veins were smooth and continuous (Figure 1). In three patients who had stage III disease, lymph vessels were invisible on MRL (Figure 1). 7 (18.5%) patients had symptoms of increased lymphatic vessel patency. One of them were of stage I, 4 of stage II, and 2 of stage III. MRL of these patients were manifested by the formation of lymphatic vessel net or collateral vessels (Figures 2 and 3). Moreover, 14 (46.7%) in 30 patients who had unilateral limb oedema were revealed that contralateral limbs were also abnormal that even without patients’ notice (Figure 4).In 35 patients with lower limb lymphoedema, MRL showed the formation of lymphatic net in 7 (14.3%) patients, lymphatic dilation in the calf in 26 (74%) patients, and 9 (26%) patients with lymphangiectasis in both calves and thighs.
Discussion
In the study population, the blockage and malformations of lymphatic vessels could be detected and displayed clearly on MIP images. Most of the patients had a history of lymph node trauma. The accumulation of protein-containing fluid in the interstitium during the process of wound repair would induce lymphatic vessel thickening and fibrosis which were manifested by MRL. We also found 14 patients diagnosed with unilateral limb lymphoedema had contralateral oedema as reported previously4. Thus, MRL may benefit for the early detection and intervention of lymphoedema.Conclusion
Our study showed that MRL could provide a comprehensive visualisation of the lymphatic system, detect the location of lymphatic blockage, and facilitate surgeons with pre-operative assessment.Acknowledgements
No acknowledgements
References
1. Stanley G Rockson, Lymphedema, The American Journal of Medicine, Volume 110, Issue 4, 2001, Pages 288-295.
2. Yasunaga Y, Nakajima Y, Mimura S, Yuzuriha S, Kondoh S. Magnetic resonance lymphography as three-dimensional navigation for lymphaticovenular anastomosis in patients with leg lymphedema. J Plast Reconstr Aesthet Surg. 2021 Jun;74(6):1253-1260.
3. Soga S, Onishi F, Jinzaki M, Mikoshi A, Minabe T, Shinmoto H. Analysis of collateral lymphatic circulation in patients with lower limb lymphedema using magnetic resonance lymphangiography. J Vasc Surg Venous Lymphat Disord. 2021 Mar;9(2):471-481.e1.
4. Seong Jong Yun, Chang-Woo Ryu, Geon-Ho Jahng, Eui Jong Kim, Woo Suk Choi, Kyung Mi Lee, Sun Mi Kim, Usefulness of contrast-enhanced 3-dimensional T1-VISTA in the diagnosis of facial neuritis: Comparison with contrast-enhanced T1-TSE, Journal of Neuroradiology, Volume 42, Issue 2, 2015, Pages 93-98.
Figures
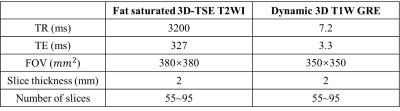
Table 1 Imaging parameters of the study cohort.
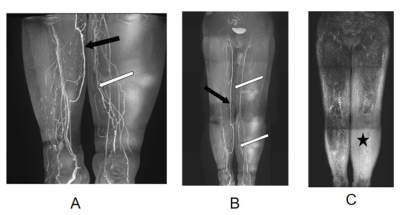
Figure 1 MIP images of patients with lymphatic blockage. White arrows denote lymphatic vessels and black arrows denote veins in (A) and (B). The star in (C) showed the disappearance of lymph vessels.
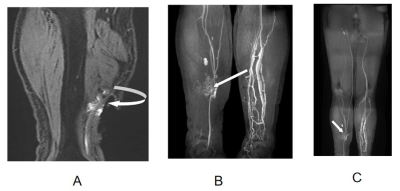
Figure 2 MIP images of patients with increased lymphatic patency. White arrows denote the occurrence of lymph vessel net.
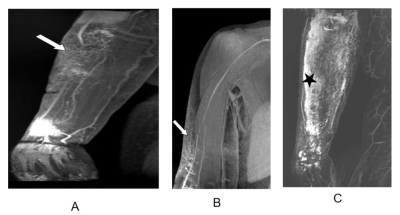
Figure 3 MIP images of patients with increased lymphatic patency. White arrows and the star denote the formation of collateral vessels.
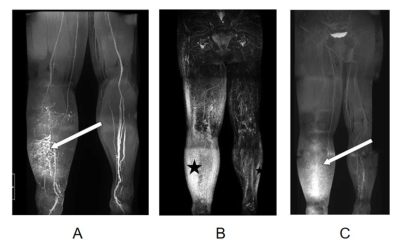
Figure 4 MIP images of patients with unilateral extremity edema reveal contralateral limb swelling. White arrows and the star denote unilateral extremity swelling sites.