4219
Quantitative evaluation of gluteal and multifidus muscle atrophy and fatty infiltration in patients with lumbosacral nerve root compression1The First Affiliated Hospital of Nanjing Medical University, Nanjing, China, 2GE Healthcare, MR Research, Beijing, P.R. China, Beijing, China
Synopsis
Keywords: Muscle, Quantitative Imaging
This study aims to investigate if MR technology can be applied to quantitatively evaluate the atrophy and fatty infiltration of gluteal and multifidus muscles in patients with lumbosacral nerve root compression. By quantitative evaluating 88 patients, we found the the change of multifidus muscle is related to the level of compressed nerve root and duration. As an indirect manifestation of nerve root compression, muscle change can help diagnosis in conventional lumbar MR images. Muscle content, especially that of multifidus is suggested to be a good indicator to complete the postoperative evaluation.INTRODUCTION
In patient with lumbosacral nerve root compression,the innervated muscles gradually show signs of chronic denervation,including atrophy and fatty infiltration1.These muscle changes reduce the strength of contraction, affecting hip joint mobility and pelvic stability, and making lower limb movement restricted2,3.Moreover, disuse atrophy may occur with the progression of limited mobility. Since conventional lumbar MR cannot show the overall shape of buttock muscles, current studies mainly focus on the paravertebral muscles. The objectives of this study were to (1) investigate side-to-side changes of gluteal and multifidus muscles in patients with unilateral lumbosacral nerve root compression, (2) investigate the correlation between muscular changes and symptom duration,and(3)investigate the muscle changes at different compression levels and the relation ship with Japanese Orthopedic Association(JOA) score.METHODS
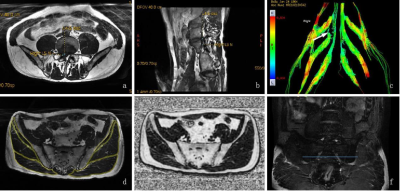
Subjects Patients diagnosed with unilateral lumbar nerve root compression were recruited.The detailed inclusion criteria were (1) low back pain with unilateral radiation pain in the lower extremity; (2 )positive Lasègue sign on the affected side; (3) complete MR images of the lumbar spine; (4) unilateral nerve root compression associated with disc herniation confirmed by MRI. The exclusion criteria were (1) previous history of spinal surgery; (2) spinal and lower extremity trauma,infection or neoplastic lesions; (3) lumbar spondylolisthesis; (4) lumbar scoliosis; (5) history of central nervous system diseases; (6) history of chronic underlying diseases. Eighty-eight consecutive patients and seventy healthy volunteers were enrolled, and their general information,including age, gender and symptom duration of patients, were recorded for analysis. Functional performance was evaluated using JOA score. MRI imaging protocol MRI of the L-spine was performed with a 3-T MR system (Discovery 750w,GE Healthcare). Three dimensional fast imaging empolying steady-state acquisition with phase cycling(3D-FIESTA-C) imaging (repetition time/echo time [TR/TE] 5.1ms/min full, slice thickness 1.4 mm, matrix 384 × 256, field of view [FOV] 400 × 400 mm) and iterative decomposition of water and fat with echo asymmetry and least-squares estimation quantitation(IDEAL-IQ) imaging (TR/TE 9.1ms/min full, slice thickness 1.4 mm, matrix 160×160, FOV 340 × 340 mm) were performed in the axial plane. Diffusion tensor imaging was employed(TR/TE 6000/80ms,slice thickness 4mm,matrix 96 × 128,FOV 420 × 420mm).The corresponding scan time was 3min58s. Data analysis Image measurement were conducted on GE ADW4.6 workstation by two trained radiologists and averaged. On axial 3D-FIESTA-C images and the fat fraction images of IDEAL-IQ squence,the cross sectional area(CSA) and fat fraction(Ff) of bilateral multifidus muscles at the L5 inferior endplate level, were measured respectively.The CSA and Ff of bilateral gluteus maximus,gluteus medius,gluteus minimus were measured at the S1 inferior endplate level,as well as subcutaneous fat area(Sfs) and thickness(Sfd). Statistical analysis Statistical analysis was performed using SPSS version 25.0 (IBM software). In the healthy volunteers group,to reveal the correlation between bilateral average CSA and Ff, and age, and sex, Pearson’s correlation coefficient was calculated. The same analysis was also applied to analyse the correlation of Sfs and Sfd to Ff.The side-to-side difference in CSA and Ff was compared using paired t tests. CSAm was used to represent the muscle content.It was calculated by the formula CSA*(1-Ff).CSAmr was defined as the ratio of bilateral muscle CSAm.The correlation between CSAmr and JOA scores was analyzed using Pearson correlation analysis.RESULTS
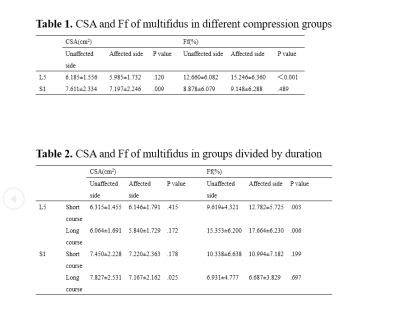
The ratio of CSA(CSAr) of gluteus maximus,gluteus medius,gluteus minimus,and multifidus muscle in the case group was smaller than in the control group(P<0.001),and The ratio of Ff(Ffr) was greater(P<0.01).There was no difference in CSA of bilateral multifidus muscle in L5 short course and long course groups, however, the difference in Ff of multifidus muscle in both groups was statistically significant (P < 0.01).No bilateral difference of multifidus CSA was showed in short course of S1 patients , but there was a significant difference in the long course group (P < 0.05).The ratio of muscle content(CSAmr) of gluteus maximus, gluteus medius, gluteus minimus and multifidus were correlated with Japanese Orthopedic Association(JOA) scores(P<0.001).DISCUSSION
After analyzing the muscles in patients with single segment nerve root compression, we concluded that the multifidus changes were related to the segment of compressed nerve roots. Previous studies have been controversial in the changes of multifidus CSA and Ff. Previous studies reported no correlation between multifidus atrophy and nerve root compression4. Other studies showed that both multifidus atrophy and fat infiltration were correlated to lumbar disc herniation5-7. In addition to different research methods, our results explain part of this controversy. Our study also emphasized a reliable fat quantitative method to evaluate multifidus atrophy and fat infiltration. By using the parameter of CSAmr, we achieved an accurate evaluation of the actual functional part of muscles and concluded the correlation between muscle content and the severity of patients’ clinical symptoms. Among the measured muscles, the CSAmr of multifidus was most highly correlated with JOA score. Thus, CSAmr of muscles, especially that of multifidus, could be a better parameter for clinical evaluation.CONCLUSION
The change of multifidus muscle is related to the level of compressed nerve root and duration.As an indirect manifestation of nerve root compression,muscle change can help diagnosis in conventional lumbar MR images.Muscle content,especially that of multifidus,is suggested to be a good indicator to complete the postoperative evaluation.Acknowledgements
No acknowledgements.References
[1]Tarulli AW, Raynor EM. Lumbosacral radiculopathy. Neurol Clin. 2007 May;25(2):387-405. doi: 10.1016/j.ncl.2007.01.008.
[2]Khedr EM, Fawi G, Abbas MA, El-Fetoh NA, Zaki AF, Ahmed MA, Soliman RK, Gamea A. Prevalence of cervical and lumbosacral compressive radiculopathies in Qena governorate/Egypt: Population-based survey. Clin Neurol Neurosurg. 2018 Dec;175:112-120. doi: 10.1016/j.clineuro.2018.10.003.
[3]Zhao WP, Kawaguchi Y, Matsui H, Kanamori M, Kimura T. Histochemistry and morphology of the multifidus muscle in lumbar disc herniation: comparative study between diseased and normal sides. Spine (Phila Pa 1976). 2000 Sep 1;25(17):2191-9.
[4]Geiringer S. Anatomic localisation for needle electromyography. 2nd edn. Philadelphia: PA:Hanleyn & Belfus; 1999.
[5]Russo M, Deckers K, Eldabe S, Kiesel K, Gilligan C, Vieceli J, Crosby P. Muscle Control and Non-specific Chronic Low Back Pain. Neuromodulation. 2018 Jan;21(1):1-9.
[6]Farshad M, Gerber C, Farshad-Amacker NA, Dietrich TJ, Laufer-Molnar V, Min K. Asymmetry of the multifidus muscle in lumbar radicular nerve compression. Skeletal Radiol. 2014 Jan;43(1):49-53.
[7]Park MS, Moon SH, Kim TH, Oh J, Lee SJ, Chang HG, Shin JH. Paraspinal Muscles of Patients with Lumbar Diseases. J Neurol Surg A Cent Eur Neurosurg. 2018 Jul;79(4):323-329.[8]Hofste A, Soer R, Hermens HJ, Wagner H, Oosterveld FGJ, Wolff AP, Groen GJ. Inconsistent descriptions of lumbar multifidus morphology: A scoping review. BMC Musculoskelet Disord. 2020 May 19;21(1):312.
Figures