4212
Quantification of lumbar paraspinal muscle injury in patients with low back pain using intravoxel incoherent motion diffusion weighted imaging
Yinqi Liu1, Weiyin Vivian Liu2, and Kun Zhang1,3
1Department of Radiology, First Affiliated Hospital of Hunan University of Chinese Medicine, Changsha, China, 2MR Research, GE Healthcare, Beijing, China, 3College of Integrated Traditional Chinese and Western Medicine, Hunan University of Chinese Medicine, Changsha, China
1Department of Radiology, First Affiliated Hospital of Hunan University of Chinese Medicine, Changsha, China, 2MR Research, GE Healthcare, Beijing, China, 3College of Integrated Traditional Chinese and Western Medicine, Hunan University of Chinese Medicine, Changsha, China
Synopsis
Keywords: Muscle, Diffusion/other diffusion imaging techniques
Chronic low back pain (CLBP) has been reported to be associated with lumbar paraspinal muscles injury. Lumbar paraspinal muscles injury may result from oxidative stress and inflammation. In our study, D* at the middle of L4 and L5 levels of the paraspinal muscles was significantly higher in LBP group than in HCs. The fluid oozing from the inflammation can lead to greater unrestricted molecular movement. Therefore, non-invasive and contrast-agent-free IVIM could be a good perfusion predictor of lumbar paraspinal muscle injury.Introduction
Chronic low back pain (CLBP) is referred that pain, muscle tension and stiffness accompanied with or without radical pain of low extremity for over three months. Chronic low back pain is one of the most common and expensive medical problems; few treatments are proven to be effective1. Agten et al. reported that chronic low back pain was the most common cause of disability in Western Europe among 291 diseases 2. Many studies have indicated that CLBP is associated with paraspinal muscle injury, but the cellular or molecular mechanism of its damage remains unclear3. Oxidative stress and inflammation may affect molecular conditions during muscle injury. Intravoxel incoherent motion (IVIM) is a non-invaisve magnetic resonance imaging technique that extracts local perfusion and also diffusion information from a multi-b-value diffusion-weighted imaging sequence, and can be used for quantitative muscular perfusion imaging4. IVIM has been rarely used to quantitatively assess muscle injury in inflammatory myopathy5. Therefore, this study aims to evaluate the feasibility of IVIM to quantify injury degree of paraspinal muscles and to compare blood perfusion differences of lumbar paraspinal muscle between patients with low back pain and healthy controls (HCs).Materials and Method
17 patients with LBP and 17 HCs underwent lumbar spine examination using routine MRI and IVIM imaging (Details in Table 1) on 3.0T MR scanner (Signa HDxt, GE Healthcare). Regions of interest (ROIs), including the middle level of L4 and L5 of the lumbar paraspinal muscle, were delineated on the IVIM maps (Figure 1). IVIM data were transferred to GE advanced workstation and analyzed to generate the average perfusion fraction (f), pseudo-diffusion coefficient (D∗), and diffusion coefficient (D) in the ROI (Figure 1). Independent samples t-test or Mann-Whitney test was used to analyze difference of IVIM parameters between two groups according to data normality and equality of variance.Results and Discussion
D* at the middle of L4 and L5 levels of the paraspinal muscles was significantly higher in LBP group than in HCs (F = 8.096, P < 0.05, Figure 2). No significant difference of D and f between two groups was found( P > 0.05). Severe muscle degeneration, inflammation, and decreased blood vessels are commonly observed in biopsies of people with lumbar lesions compared to normative data 6. Many studies have confirmed that paraspinal muscle inflammation can lead to the increase of IL-1β, tumor necrosis factor and IL-107. Since inflammation involves fluid infiltration, a larger extracellular space and less membrane barrier are formed, allowing for greater unrestricted molecular movement5.Conclusions
Our study showed D* of the lumbar paraspinal muscles was significantly increased in CLBP patient. That is, D* represents intravascular blood flow and can quantify lumbar paraspinal muscle injury in CLBP. IVIM parameters may offer adjunctive information about CLBP, and its clinical role needs further validate in future larger-sample study.Acknowledgements
Funding: None.References
- Russo, M., et al., Muscle Control and Non-specific Chronic Low Back Pain. Neuromodulation: Technology at the Neural Interface, 2018. 21(1): 1-9.2.
- Agten, A., et al., Biopsy samples from the erector spinae of persons with nonspecific chronic low back pain display a decrease in glycolytic muscle fibers. Spine J, 2020. 20(2): 199-206.3.
- Shahidi, B., et al., Lumbar multifidus muscle degenerates in individuals with chronic degenerative lumbar spine pathology. Journal of Orthopaedic Research, 2017. 35(12): 2700-2706.4.
- Le Bihan, D., What can we see with IVIM MRI? Neuroimage, 2019. 187: 56-67.5.
- Qi, J., et al., Diffusion-weighted imaging of inflammatory myopathies: Polymyositis and dermatomyositis. Journal of Magnetic Resonance Imaging, 2008. 27(1): 212-217.6.
- Wang, X., et al., Research Progress on the Mechanism of Lumbarmultifidus Injury and Degeneration. Oxidative Medicine and Cellular Longevity, 2021. 2021: 1-9.7.
- Hodges, P.W., et al., Can proinflammatory cytokine gene expression explain multifidus muscle fiber changes after an intervertebral disc lesion? Spine (Phila Pa 1976), 2014. 39(13): 1010-7.
Figures
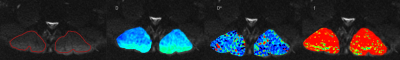
Figure 1 ROIs of the lumbar paraspinal muscle and representative parameters maps of perfusion fraction, D, D* and f for a 37-year-old male paitent with CLBP .
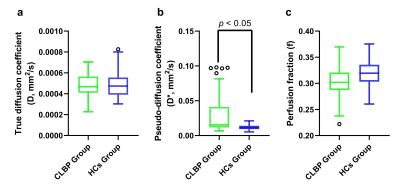
Figure 2 Boxplots of IVIM parameters: D(a), D*(b), f(c). D* at the middle of L4 and L5 levels of the paraspinal muscles in CLBP group (mean 0.03055±0.004518 mm2/s) was significantly higher than those in HCs group (mean 0.01207±0.0005784 mm2/s) (as assessed with t-test with p < 0.05).
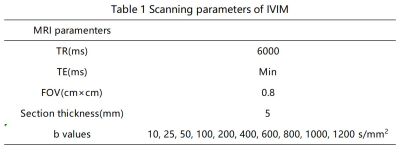
Table 1 Scanning parameters of IVIM
DOI: https://doi.org/10.58530/2023/4212