4195
Clinical assessment of a deep learning-based denoising method for DWI of Nasopharyngeal Cancer
Tiebao Meng1, Haibin Liu1, Haoqiang He1, Jialu Zhang2, and Long Qian2
1Department of Radiology, Sun Yat-Sen University Cancer Center, Guangzhou, China, 2MR Research, GE Healthcare, Beijing, China
1Department of Radiology, Sun Yat-Sen University Cancer Center, Guangzhou, China, 2MR Research, GE Healthcare, Beijing, China
Synopsis
Keywords: Machine Learning/Artificial Intelligence, Diffusion/other diffusion imaging techniques
Deep Learning reconstruction (DLR) has the potential to reduce MRI scan time while improving signal-to-noise ratio (SNR) and maintaining spatial resolution. This study evaluated results of DLR in 66 patients undergoing clinical DWI of nasopharyngeal cancer (NPC). To assess the image quality of the DWI with DLR, each patient underwent three different protocols: conventional DWI without DLR, fast DWI without DLR and fast DWI with DLR. The image quality was evaluated among these groups. Preliminary results suggested the feasibility of fast DWI with DLR in the diagnosis of NPC with reduced scan time.Introduction
Nasopharyngeal cancer (NPC), as a frequently reported incidence of otorhinolaryngology, requires excellent diagnostic accuracy in every stage1. Diffusion weighted imaging (DWI) has been an essential method for NPC diagnosis due to its unique contrast with lesions. However, EPI-based DWI methods with single number-of-excitation (NEX) could commonly suffer from limited image signal-to-noise ratio (SNR). Although high-quality images can be obtained with more NEX, it would prolong the scan time of patients. Deep learning-based reconstruction (DLR) has been proven as a novel approach to settle the dilemma by providing promising image quality within single scan2, 3. In this study, each patient underwent three different protocols of DWI: conventional DWI without DLR, fast DWI without DLR, fast DWI with DLR. Different measures of image quality were assessed and compared among these three groups.Methods
From May to October 2022, sixty-six patients with NPC were examined and diagnosed on a GE SIGNA Premier 3T MRI scanner under an IRB-approved protocol with written informed consent. Each patient underwent three different protocols of DWI sequence with single-shot EPI acquisition. Two b-values, 50 and 800 s/mm2, were scanned with different NEX and DLR conditions: (1) Group1 (G1), conventional DWI without DLR, NEX = 2, 6 (for each b-value); (2) Group2 (G2), fast DWI without DLR, single NEX for each b-value; (3) Group3 (G3), fast DWI with DLR, single NEX for each b-value. All protocols acquired with the same other parameters as follows: TR = 2600 ms; TE = minimum; slice sickness = 5 mm with 1 mm spacing; FOV = 24 cm; image matrix = 128 × 128; a total time of G1 was 1 min 12 sec, G2 was 27 sec, and G3 was 27 sec.The apparent diffusion coefficient (ADC), SNR and contrast-to-noise ratio (CNR) in region-of-interest (ROI) were calculated for objective evaluation of image quality. The assessment of overall image quality and lesion conspicuity were made using a standardized 5-point Likert scale4 by two independent oncologists. Statistical analyses were performed using repeated measure ANOVA test with Bonferroni correction. For all tests, p < 0.001 was considered as statistically significant.Results
The results of different protocols from a typical patient were presented in Figure 1. The image from fast DWI with DLR showed a higher ADC in lesion area (red ROI) giving more detailed metabolic information in tumor. Table 1 showed the values of ADC, SNR and CNR from different groups, representing the objective image qualities of each DWI protocol. As demonstrated, significant differences of SNR and CNR values were detected and there was no between-group difference of ADC values. The pairwise comparisons of each two protocols were shown in Table 2. As expected, fast DWI with DLR showed significant increased SNR compared to fast DWI without DLR. Moreover, compare with conventional DWI without DLR group, the fast DWI with DLR had similar SNR, CNR and ADC values. Table 3 exhibited the averaged qualitative image quality scores given by different oncologists. It was shown that fast DWI with DLR obtained a significantly improved image quality compared with fast DWI without DLR and had comparative scores with conventional multiple averaged DWI results.Discussion and conclusion
In this study, the comparison between images of different fast DWI protocols demonstrated that DLR technique can significantly increase the image quality of DWI images from NPC patients. Moreover, it was shown that the fast DWI protocol with DLR was proved to have similar image qualities and comparative ADC values compared with conventional multi-NEX DWI protocol. Thus, it is feasible for further clinical applications of fast DWI protocol in the diagnosis of NPC with reduced scan time.Acknowledgements
No acknowledgement found.References
1. Lai, Vincent, and Pek Lan Khong. "Updates on MR imaging and 18F-FDG PET/CT imaging in nasopharyngeal carcinoma." Oral oncology 50.6 (2014): 539-548.
2. Hahn, Seok, et al. "Image quality and diagnostic performance of accelerated shoulder MRI with deep learning–based reconstruction." American Journal of Roentgenology 218.3 (2022): 506-516.
3. Sreekumari, A., et al. "A deep learning–based approach to reduce rescan and recall rates in clinical MRI examinations." American Journal of Neuroradiology 40.2 (2019): 217-223.
4. Joshi, Ankur, et al. "Likert scale: Explored and explained." British journal of applied science & technology 7.4 (2015): 396.
Figures
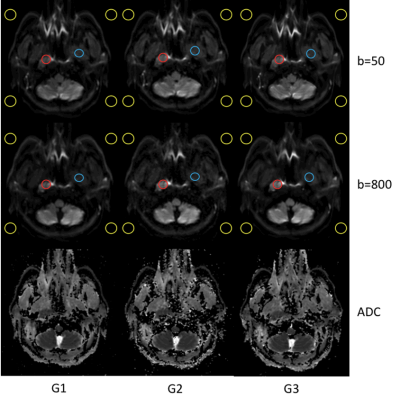
Figure 1. The ADC comparisons of one patient for three DWI protocols. The red, blue and yellow circles were respectively represented the ROIs of lesion, normal tissue and noise for objective evaluation of image quality.
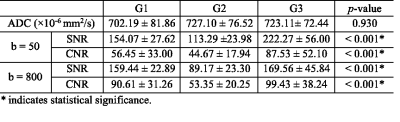
Table 1. Comparison of objective image qualities for three DWI protocols.
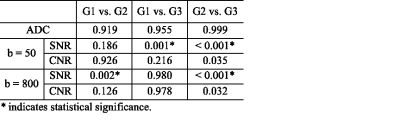
Table 2. Pairwise comparison of objective image qualities for three DWI protocols.
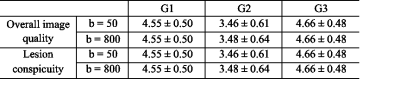
Table 3. Comparison of image quality related scores for three DWI protocols.
DOI: https://doi.org/10.58530/2023/4195